
Thanks for supporting our Global Giving Day
![]() Ian Robinson
Ian Robinson
![]() 25th August 2020
25th August 2020
To our friends and supporters,
Thank you so much for your support in various ways that has enabled us at PcERC and MMPCU Uganda to continue to provide care to our patients and their families during this period. We have now raised $2,000 out of our $7,500 goal since the campaign started 7 weeks ago on Global Giving. (https://www.globalgiving.org/)
We remain grateful to you who have supported us thus far and those who will be supporting us in future.
Global Giving has now announced the July Bonus day which is a one-day campaign aimed at helping us to secure larger donations for our project.
So come Wednesday 15th July 2020 Global Giving will match all donations of $100-$1,000 as well as other award prizes!
Donations will be matched based on amount:
Donations of $100 - $499 USD will be matched at 15%
Donations of $500 - $749 USD will be matched at 30%
Donations of $750 - $1,000 USD will be matched at 50%
We are therefore calling upon you once again to come and support us on this day in whichever way you can. Please click on this link; https://www.globalgiving.org/projects/covid-19-bringing-hope-through-palliative-care/. You can donate as a one-off or monthly.
Also our normal Bringing Hope through Palliative Care project is still running where you can still give as a one off or regularly. Please click on the following link; https://www.globalgiving.org/projects/reducing-suffering-palliative-care-in-uganda/
With best wishes and blessings
# stay safe
MMPCU/PcERC team

A new experience for the Gathering in 2020
![]() Cairdeas
Cairdeas
![]() 25th August 2020
25th August 2020
Due to the COVID-19 lockdown, we decided that this year we would hold our annual gathering on line via Zoom. This gave us a great opportunity to welcome some of our partners and supporters, who would otherwise be unable to travel to Scotland, to join us.
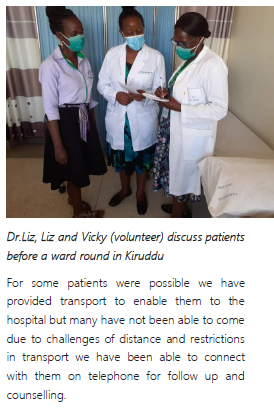
We had an enjoyable afternoon on Saturday 27th June meeting up with each other and learning about what Cairdeas has been up to since we all met last year. Invited speakers were Dr Chitra Venkateswaren from the MEHAC Foundation talking to us about how they are adapting palliative care principles for the treatment of COVID-19 patients in India, Elizabeth Namukwaya updated us on the work of PcERC and MPCU in Uganda. Dr Elizabeth Swain talked about her visit to Gaza and the Palliative care conference for Palestine. Sarah Robinson and Vicki Opia told us about the work of the Peace Hospice in Adjumani district and Sarah’s visit there last summer.
Dr Mhoira Leng, our Medical Director gave an update on the ongoing work of Cairdeas during this last year and how it has been impacted by the COVID-19 pandemic.
We also introduced our new Operations director, Ian Robinson, who joined us in May.
For part of the afternoon, we were able to break off into breakout rooms to chat in smaller groups which enabled us to meet some of our partners in person as well as each other.
The afternoon was recorded on video, which you can find in the resources section of the website for anyone who missed the Gathering to catch up, or for anyone who wants to recap on the talks.

An opportunity to meet some of our partners from Uganda and India and welcome them to our annual gathering
Welcome to our new Operations Director UK
![]() Cairdeas
Cairdeas
![]() 25th August 2020
25th August 2020
We are delighted to announce that Ian Robinson has recently been appointed as our new UK Operations Director. Ian takes over from Sarah Robinson who has served faithfully over the last 18 months. We’d like to take this opportunity to thank Sarah for all the work that she has done for Cairdeas over the time she has been with us.
Ian recently retired from a long career as a chartered electrical engineer. He has worked on project work in the UK and overseas for heavy industries. He has also in recent years run his own consultancy business and brings skills in this area to our operation.
Ian has also been a volunteer for various organisations for many years. For quite a long time he has volunteered as a befriender for Care for the Family’s Bereaved Parents Support network and has also been involved in fund raising for the Brain Tumour charity, Hope for the Future, Parkinsons UK and the Mustard Tree Trust (Northumberland).
Ian is interested in music and plays in Morpeth community Jazz Orchestra. He is also a keen runner and was due to run in the Great North Run this year. Ian is a keen Sunderland supporter.

