
Transform Obongi and Adjumani; supported by UKAID
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 31st March 2021
31st March 2021
We were delighted to be awarded one of the UK government #smallcharitieschallengefund grants in February and are busy working with our partners, Peace Hospice Adjumani and the Palliative care Education and Research Consortium in Uganda to get the maximum benefit for the people of Obongi and Adjumani districts. Our grant official title is 'Empowering communities and health systems to address health related suffering in host and humanitarian settings through capacity building and integration’ and will focus on understanding the experience of those living with health-related suffering and working with community and health leaders to build capacity and improve care. We are building on a previous work with the same partners alongside the Ministry of Health which focussed on Adjumani District only.
Uk Minister for Africa James Duddridge said: “I am delighted that Cairdeas is using the UK Government’s Small Charities Challenge Fund to be a force for good in the world by helping some of the world’s most vulnerable people. “We are committed to supporting Uganda’s ongoing development, while providing urgent, life-saving humanitarian support to refugees and those in the greatest need in the country.”
Obongi and Adjumani are both districts in the North of Uganda bordering the river Nile. They are close to the South Sudan border, a country that has seen decades of conflict before gaining independence from Sudan in 2011 and then a grinding and brutal civil war. Refugees have fled and many have found a welcome in Uganda, one of the countries with the highest levels of refugee and migrant populations. This has not just been a government policy of welcome but has also been reflected in the local population of the neighbouring areas...which also include the Democratic of Congo where repeated conflict drives refugee numbers. There is much to learn about how refugee as seen as brothers to these rural, poor populations that are rich in humanity and where there is 1 refugee to every 2 host population in overall numbers yet little conflict.
Over the next 2 years we will share experiences of working together and some of the people we meet and places we visit. Let me take you on a virtual visit to whet your appetite....drive with me many km from Kampala to the town of Gulu and then turn onto mostly dusty murram road till we reach the town of Adjumani and the warm welcome from our lead partner and friend Vicky Opia and her husband Solomon. We still have further to travel including crossing the mighty White Nile river to get to the district of Obongi. Already we have journeyed for 7 hours or so and it’s time to rest and eat amazing yams, fish from the lake, mangoes from the garden, sweet sim sim balls or whatever delights Vicky has prepared for us.... all to the accompaniment of Solomon’s choice of Congolese music.
Peace Hospice and the local Ministry of Health hospitals and clinics as well as the additional capacity for refugees supported by UNHCR and Medical Teams International have responded to the increased need. The one District Hospital in Adjumani which was without even basic x-ray and ultrasound is now better equipped and other smaller clinics are being developed into hospitals. The palliative care teams here started responding in a ground-up way to the needs. They took to their available transport...motorbikes...and travelled deep into the countryside faces tightly wrapped against the dust. They worked to find those in need and either bring them to the hospital or offer support at home. Peace Hospice was the only team doing home care and Vicky is the District lead for palliative care within the Ministry of Health and the Refugee joint health sector meetings. We have previously supported her to train health care workers in the hospitals and health clinics across Adjumani district. Our projects have all grown out of this amazing work on the ground and work closely with the community and health leaders. There is good news that the previous DHO for Adjumani is now an MP in Obongi. Dr...will bring his wisdom to his new role I am sure but he is also very aware of the need for palliative care. He was pleased we showed the level of need in our last piece of work and keen we extend this to the host population so we will eb carrying out another piece of research to identify people living with chronic illness at village level and find out the extent of their need. This time we will be delving deeper into their experience of distress since so many are suffering the effects of chronic trauma.
Key to any community change is local initiatives and leadership. We will be training family members and village health teams but also listening to them and finding out the realities of their situation and the ways they have found to address their needs. This ground up approach is crucial and ensure we will all be learning. WE will be using interviews, photographs, mentoring and home visits as we seek to understand more deeply and help design training and research to build capacity and improve the care. This work will have relevance far beyond this setting.
What reception will we get? I have experienced the warm, openhearted nature of so many despite the many challenges of daily life. Problem solving and imaginative use of scarce resources is a way of life. The Governmental and non-governmental organisations do realise the problem of chronic illness and are seeking to meet the needs but lack evidence for planning, needs more trained workers and also want guidelines and processes. The latter links with national work between the MOH and the Palliative Care Association of Uganda to develop a national roll out of information systems and palliative care services. We will be seeing how the health system is managing thus far.
Palliative care in humanitarian settings is increasingly being recognised as woefully inadequate and requires cross sectoral working and crucially ground up approaches. PallCHASE is a global network seeking to raise awareness and develop support systems for improving access to quality palliative care in humanitarian settings and I am delighted to be serving on their executive. I know the work from the Transform Obongi and Adjumani will help shape and inform global initiatives. Please look out for the first in a new series of webinars from PallCHASE to be announced soon.
Lastly, let me share the words of the nursing officer at Adjumani hospital. She was honest that she was unaware of the scope of palliative care and left it to Vicky. However, after seeing her staff trained and hearing from families about the impact, she changed her mind completely. She said '‘Someone needs to speak for the voiceless. When help comes, people change. It is like losing hope — then hope appears suddenly like the sun.’
Bringing hope, bringing joy and always learning more about our common humanity.
For more information see www.cairdeas.org.uk
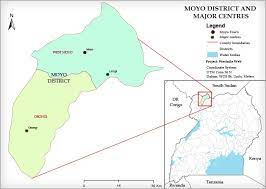
Obongi district..Adjumani just across the Nile

Sam, Peace Hospice nurse, on his bike is a kid magnet

Sam on home visits; communal and cross generational

Crossing the Nile...there is a ferry for more regular use

Vicky and one of her previous patients, Aneurina

Mangoes in the garden

Fresh fish is a treat

Brick making in the village

Off grid so solar panels on sale in Adjumani town

Water pumps...so essential

Refugee village
Shared vulnerability, one humanity with kindness
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 3rd December 2020
3rd December 2020
Unusually for this time of year I am in Scotland and this morning has a wonderful frosty walk up Blackford Hill in Edinburgh. In the early morning half light passers by, many with excited dogs careering around, greeted each other and said 'is it not beautiful' and 'I'm so lucky to see this sunrise'. The joy of sharing unexpected beauty with stangers.
So many are seeing 2020 as a year to write off, to 'coorie down' under the blanket of snow and of too many challenges and losses and hardships. Many of you will have experienced so much loss and grief, fear, distress and now simply feel overwhelmed. For many these challenges will move into the next year as the impact of the COVID-19 pandemic and what is being called the syndemic of the health care and economic problems carry over and may even increase. This has been a time of global challenge yet it has not affected people equally. Our health systems in the UK and other high income places have been almost overwhelmed but what of places where the basics of health care are a challenge. We may have had more than a glimpse into these realities. In the far north of Uganda Vicky Opia has been working in a critical area with rural populations, refugees and migrants and border movements that have led to a high COVID-19 incidence. In Kampala, COVID-19 numbers were slow to rise but are peaking now but what of the numbers needing cancer treatment or even basic food when your daily wages have been lost or struggling to work in the midst of a oandemic without PPE or safe transport; thansk to the PcERC team for all they do (see earlier blog). India with so much to give this world has struggled to manage the impact of COVID-19 on it's huge and diverse population. Think of our brothers and sisters in Gaza, trampled and constrained by 13 years of siege and lockdown, and now with COVID-19 numbers rising and health systems collapsing. We have also seen amazing global solidarity as we sought to face this pandemic together and learn much more about what it means to be truly global citizens. I have shared this before but it still rings with hope; an editorial by Lukas Radbruch et al in The Lancet in April said ' The call to fully incorprate palliative care into global health could finally be realised in the urgency of this pandemic. If so the COVID-19 pandemic will have catalysed medicine to better alleviate suffering in life and death.'
In palliative care we journey each day with those who face grief and loss at a personal level and together seek to find strength, courage and hope...while facing our own powerlessness and vulnerability. How do we hold these places of uncertainty and challenge? Where do we go to find meaning and hope? For each of us this will mean different things as we reach out to our places of resilience and strength or find new ways of making sense of life. I have so appreciated a daily Northumbrian Celtic prayer cycle with a group of like minded people to centre and reflect each day. We need those places of stillness and openness to one another. I was discussing on a webinar recenlty the incredible thread of our common humanity throughout this historic year and my colleague from South Africa explained he has learned that it is in those places of shared vulnerability we see our common humanity. Our training programme with PalliCOVIDKerala and Pallium India (see earlier blog) has been a place where people shared their vulnerabilities; at times up to 100 people from across many states and countries yet finding and holding those places together. One saying 'I will be more compassionate to the patients and high risk groups and to myself'. Some of our Cairdeas Faculty have been teaching in a new programme with Mercy Ships and we have seen people really thirsty to learn even if internet, civil unrest, monsoon rains and a myriad of other challenges got in the way. Our IUG medical students, whom we sadly only met online in Gaza spoke of the values that were important to them #empathy #dignity #listening #hope #trust #kindness with one student saying 'we will be as you think of us'
If we are to be vulnerable then we need to know we will be met with kindness. We have seen extraordinary and simple acts of kindness. From top chefs changing their restaurants into free food for key workers, to makeshift kitchens to feed migrant workers...from rainbows in windows to music played outside hopsital windows and in lockdown streets.to neighbours caring for the vulnerable person in their community and faith groups finding new ways to reach out to those most in need when unable to gather together. We have seen innovative and imaginative ways to share love and care and have realised how much we took a simple hug for granted.
As this year draws to a close I wanted to share some of the images of beauty and kindness that have touched my heart this year. We go into a New Year with stillness and hope to embrace the many new opportunities opening up and the joy of working with partners accross the world in a common vision. Here is a beautiful blessing attributed to Theresa of Avila who lived in the 16th century and which I have been reading in the middle of each day this year. 'Let nothing disturb thee, nothing affright thee; all things are passing, God never changeth! Patient endurance attaineth to all things; who God possesseth in nothing is wanting; alone God sufficeth.'

Sunrise in Edinburgh

Path to the unknown in Skye

Vicjy and her team, Adjumani

Bringing hope, bringing joy

Indian conference in Guwahati in February

Teaching with Mercy Ships

Islamic University students and Faculty

Sharing a Palestinian meal

Kindness
Hello and thank you for your support
Cairdeas
![]() 3rd December 2020
3rd December 2020
Hello all, I thought it was about time that I introduce myself to the Cairdeas community! I’m Sophie, a university student from the North-East, and I’ve been doing some of Cairdeas’ fundraising and communication work for little over a month. This year has been difficult in so many ways which is all the more reason to be proud of what has been achieved and to thank you – our supporters – for your continued support despite whatever challenges you may be facing yourselves.
Although most of us have been in lockdown, that hasn’t stopped the work. In fact, it’s more important than ever before. Countries where we work are facing huge economic hardship. Recently, we were able to give a contribution to PcERC in Uganda. Even relatively simple tasks like organising transport and meetings are made 100 times more complicated in the midst of a global pandemic and we have to think of alternatives. Fortunately, Cairdeas has a car and we were able to pay for a driver and petrol for those who do not have cars and were at higher risk of contracting COVID19 on public transport. This allowed 3 of our senior nurses and clinical officers to travel safely to work and visit their patients. It has also provided the driver, Jimmy, with a much-needed source of income as like mnay on daily wages there is no support system when all your income disapears. Here is what one of our most valued and senior nurses, Florence, sharing what this has meant. 'The entire PcERC staff would like to acknowledge our funders especially Cairdeas for daily transport contribution to attend to our patients. We thank you so much for protecting us from using public transport during this Covid 19 pandemic . The majority of the Ugandans do not use SOPs especially passengers using public transport. May God Bless You'
However, there is also not-so-good news. For small international development charities like ourselves, the biggest single challenge we face is funding. Many UK funders have amended their giving criteria to only support UK-based projects and the foreign aid budget is being cut. As a small charity, it’s important that we look to the future and keep exploring all of our options. Corporate fundraising has been identified as a potential avenue. If this is something any of our supporters feel they have a link to, we would be delighted to hear from you.
If I may, I’d also like to take a minute to draw your attention to our fundraising accounts on Amazon Smile https://smile.amazon.co.uk , Give As You Live https://www.giveasyoulive.com and Easyfundraising https://www.easyfundraising.org.uk. Thousands of retailers are signed up to these websites and when you make a purchase, they give a small donation to us at no extra cost to you. It’s a simple (and free) way of raising funds which soon mount up and allow us to keep supporting our partners. Next time you shop online, please do consider using these sites (you can also find the links on the website).
We welcome donations through our website and will be focussing these on COVID-19 related expenses and needs for our partners and of course if you can committ to regular support that allows us to plan ahead. 2 of our partners also have their own Globalgiving campaigns right now so please consider donating directly and even think of becoming regular donors as they seek to build sustainability. PcERC in Uganda are seeking to bring hope through their care for patients and families https://www.globalgiving.org/projects/covid-19-bringing-hope-through-palliative-care/ and Peace Hospice Adjumani are reaching out to refugee families https://www.globalgiving.org/projects/adjumani-palliative-care-fund/
Thank you again for reading our blog posts and following our work. Your support really does make a difference and I’m sure you’ll be delighted to hear that we are planning some exciting ways to get involved in raising friends and raising funds for the coming year!
