
Beyond the Nile
![]() Cairdeas
Cairdeas
![]() 1st October 2020
1st October 2020
One major role of Palliative care Specialist is to respond to management of complex cases of severe pain and other symptoms, sometimes in difficult to access locations. This story is from Vicky Opia, coordinator of Peace Hospice Adjumani and a Palliative Care Nurse specialist.
Usually, doctors and nurses who face challenges in the management of difficult and complicated pain, call for support of a specialist. In June 2020, a doctor met a child diagnosed with Esarcoma who was in agony of pain. We did not only initiated him on Morphine, but also discussed the importance of surgery to avoid metastasis. Two days later, the boy’s right limb was amputated after his consent was sought.
John (not his real name) is the 3rd born among 5 siblings. At 4 years, his parents separated and he grow up with his grandmother. John's father derived his livelihood from fishing to support the family and his grandmother did the house chores. John said, ‘’My dream while in primary 2 to become a doctor came to pass when I succumbed to cancer. I experienced painless swelling at the right lower limb from 2018 which stopped me from playing and I discontinued schooling in Primary 2. I was taken for treatment at local herbalists (painful cutting with razor and massaging) and also medical care from Obongi Health Centre IV in vain." The family of seven lives in a small dwelling house and derived their livelihood from fishing and sale of labour to buy basic necessities for daily survival.
Obongi District was separated from Moyo in 2019 to bring services nearer to the community. It is 35 km from Adjumani district including 2 km across the River Nile. It has 14 health centers and 1 hospital where none of the health workers have benefited from any palliative care training. Hence they lack knowledge and skills in management of palliative care cases making them find their way to Adjumani district for services.
John and family live in a village 10 kms away from Obongi town, thus coming for review requires them to cover 45 kms in 4 hours due to ferry cross over time. Besides, the current heavy runs have flooded the roads and the river banks hence blocking access for services. The available means for transport is the local canoe.
One day, I got a call in a middle of a meeting, when I picked, it was John calling me using his father’s phone. He explained, I am in severe pain and my father cannot raise any penny to transport me for review. Immediately, I reflected on his background, my heart lept with pain and passion having known how bad and risky the road is, and particularly the pain associated with the amputation, I knelt down and prayed. The prayers empowered me and I even forgot that this river has crocodiles, and other wild reptiles. I only recalled his voice saying, ‘’Sr. Vicky am in pain……… in pain.,,, and my morphine is finished’’, Dad has gone fishing, grand mum cannot manage to carry me up to Adjumani ,please help me’’ My passion for humanity beyond self-gain, and own life disappeared. I waded in the River to save John from Severe pain. While there, 3 other patients benefitted from our services.

John (not his real name) needed urgent pain relief after an amputation

The only way to reach John's village was to wade across the river
Compassion and dignity; palliative care in COVID19 online teaching
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 15th September 2020
15th September 2020
COVID19 has altered so much in our world and emphasised the global insecurity but also the global solidarity of our interconnected world. As ever, this momentous challenge is disproporionately affecting those on the margins. We see this challenge in children unable to socially mix or go to school but also with increasing food insecurity and anxiety. We see the liminal position of refuggees and migrants widened. The plight for prisoners, those who rely on daily wages, those with pre-existing chronic illness and of course the elderly is compounded by difficulties in accessing health care services and the sense they may be pushed to the back of any treatment priority especially when resources are limited. This has been called a 'tsunami of suffering' (Radbruch L, Knaul FM, de Lima L et al. The key role of palliative care in response to the COVID-19 tsunami of suffering. The Lancet April 22 2020) where integrated palliative care has a key role in communication and goals of care, triage and symptom control, psychosocial and spiritual care, end of life care and staff support. Initially palliative care was missing from most international and national planning but we now have growing support from the WHO and from state level governments as well as many passionate individuals and organisations.
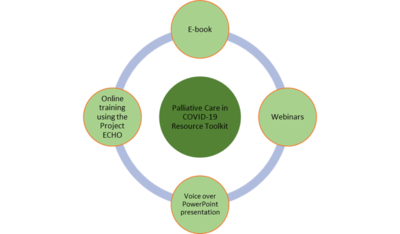
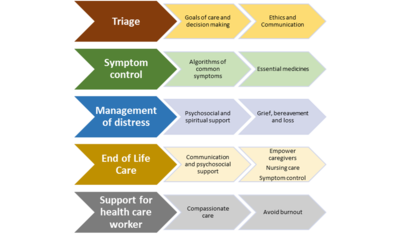
With this background a group of palliative care colleagues based in Kerala along with myself as an 'adopted Keralite' formed PaliCOVIDKerala and started to plan how we could support and empower health care workers caring for seriously ill patients and families in Low and Middle Income Countries (LMIC). Our focus were the key areas where palliative care contributes as part of COVID-19 management approaches;
- those who are COVID-19 positive and are deteriorating despite interventions
- those with pre-existing co-morbidities impacting on treatment decisions
- needs of the wider community including health care workers as they address the challenges of those affected by the COVID-19 pandemic
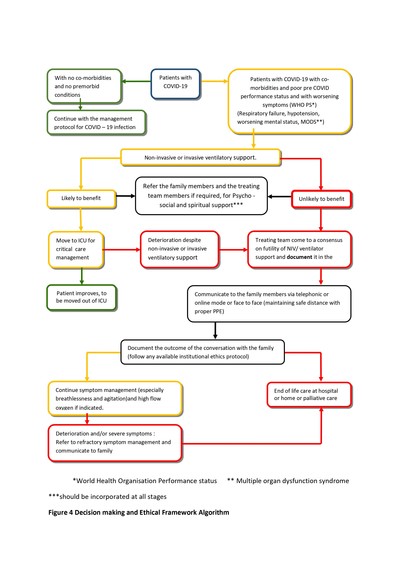
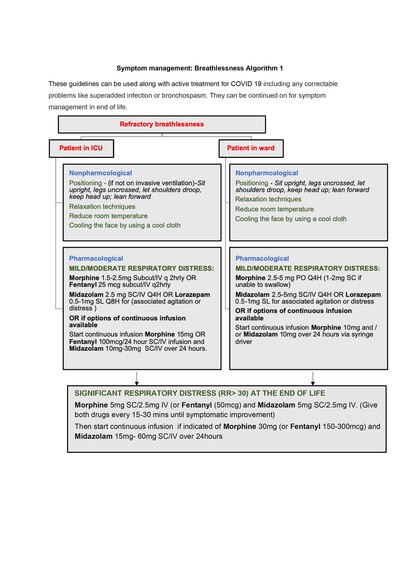
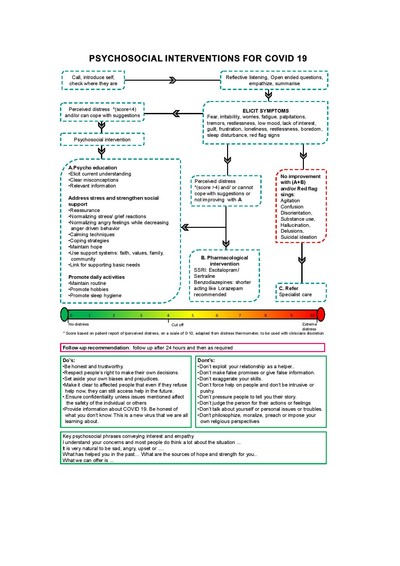
This has been an amazing journey. Our Faculty group is an important place for mutual encouragement and support and has expanded to include colleagues across India and internationally. We developed an open access e-learning programme based on 10 competencies that includes an e-book (now in the 3rd review process), 9 webinars from experts and a 5 session ECHO-India platform interactive course hosted by and partnered with Pallium India. https://palliumindia.org/2020/06/resources-for-palliative-care-in-the-context-of-covid19. We developed 11 algorthims to support practice for areas such as triage or managing distress. This format allows flexible learning where people access the sections most relevant to them and can adapt or adopt the learning in their settings. Our developments have been published in the Indian Journal of Palliative Care and Prof Chitra Venkateswaran will share more about this training in the upcoming EAPC Research conference online.
Daniel, Sunitha & Venkateswaran, Chitra & Sunder, Poornima & Nair, Shoba & K C, Rajashree & Manuel, Athul & Raghavan, Biju & Mm, Sunilkumar & Rijju, Vineetha & Vijay, Geetha & Rao, Seema & Prabhu, Anupama V & Parameswaran, Uma & Spruijt, Odette & Rajagopal, M. & Leng, Mhoira. (2020). Responding to Palliative Care Training Needs in the Coronavirus Disease 2019 Era- The Context and Process of Developing and Disseminating Training Resources and Guidance for Low- and Middle-Income Countries from Kerala, South India. Indian Journal of Palliative Care. 26. 8-16. 10.4103/IJPC.IJPC_131_20.
I am this week helping to facilitate the 17th batch of students and feel humbled to be part of this far reaching initiative. We have supported more then 700 health care workers from a range of disciplines directly through these courses from 10 countries including 25 states in India with 4 now having mandated this training by state governments. Many more have accessed and used the training materials in their own settings including translation in Bangla. This has included HCWs in rural areas such as Uttarakhand and Mizoram sharing mutual learning with those from Ghana and the Philipines...showing the opportunity we have from online learning. It has also become a safe place for us to think deeply about care with compassion and dignity, the importance of presence and value for each person, the need for effective communication and to address fears and concerns and the vital component of being compassionate with ourselves as health care workers.
Feel free to share this initiative and to register for one of the course via the Pallium India website.https://palliumindia.org/. We will also be posting the e-book and materials in our Cairdeas website resources section very soon. We are still to do a more formal evaluation but let me share some feedback from course participants.
'I will be more compassionate to the patients and high risk groups...and to myself'
'As a social worker I was happy to attend this course. Some of the most importnat points were communications, psychosocial and spiritual issues, grief and bereavemnet alomg with the importnace of the mental health of caregivers (us) during COVID19. We are forever grateful.'
'I came to know things that will help me serve patients more efficiently and also enhance my knowledge stock. The programme was wonderfully conducted by experts from various domains and strict time management made it smooth running. I would like to thank corresponding team for their support.'
'I learnt how to deal with the patinets with life-threatening disease and COVID-19 patinets uder palliative care with empathy, compassion and love.'
'The course in this situation is very effective for me because COVID-19 is a very new, unknown and scary situation. Training on how to handle this situation and how we talk with patients is very good and informative. Interaction sessions where we ask questions allowed us to clear out doubts'
'This program was very comprehensive and pratical. I highly recomend this to all who have an interest in inculding compassionate care in their pratice.'
Finally, this quote from a letter published with colleagues in the Lancet (Coughlan R, Leng M et al Lancet letter; Vol394 Oct 2019; Role for palliative care in advancing health in conflict settings) sums up this humanitarian approach to palliative care 'Suffering in illness and dying reminds us of the universal truth of our mortality and humanity. Palliative care is rooted in the recognition of our common suffering in illness and dying, our compassionate response to suffering, and our shared humanity. Fundamentally, palliative care seeks to ease suffering and uphold dignity'

Did you miss the 2020 Gathering?
![]() Cairdeas
Cairdeas
![]() 2nd September 2020
2nd September 2020
We held our annual gathering on line this year on the 27th June. We had over 50 people join us from around the world on line. It was great to be able to hear about the great work Cairdeas is doing and supporting in different places and to hear from some of our partners about their work. We heard from:
- Jacqui Mackintosh (deputy chair of the Trustees)
- Dr Mhoira Leng (Medical Director) about the response to COVID-19
- Dr Chitra Venkateswaran from the MEHAC Foundation (India) about the work of our India Partnerships
- Dr Elizabeth Swain and her attendance at the GAZA PalCare Conference
- Elizabeth Namukwaya, director of the Palliative Care Education and Research Consortium (Kampala)
- Vicky Opia and Sarah Robinson (former UK Ops Director) about the work in Adjumani (Uganda) of the Peace Hospice
- Ian Robinson (new UK Ops Director) on how you can support us
If you missed the gathering we have added videos of the zoom presentations from each of the speakers in the resources section of our website. You can access them via this link Cairdeas-gathering-2020
For any further information on our work, please visit our website at www.cairdeas.org.uk and follow us on Facebook and Twitter @CairdeasIPCT.
