
An update from Uganda to our dear supporters
![]() Cairdeas
Cairdeas
![]() 2nd July 2020
2nd July 2020
To our dear supporters,
Hope we are all keeping safe during these times!
We want to appreciate and thank you for responding to our appeal for financial support and prayers during this period of Covid-19. We are delighted to let you know that our patient care has continued during this period and we are happy to bring you some updates.
Access to care and support
In the month of April, we cared for 22 patients in the hospitals as well as following them up by telephone especially for those that had been discharged or those that were very far away and couldn’t make it to hospital for reviews.
The main challenge for our patients is access care and follow up during this lockdown period is transport as a result of the ban on both public and private transport, so we have supported them to meet the costs of hiring a vehicle or motorcycle to get them to hospital.
And he says …… “I am grateful for the love and care. It has given me hope and courage to complete my treatment without being worried of missing any of the treatment”
Patient AY’s ray of hope during this difficult time.
“ ….Covid 19 has robbed me of my family support, no one visits and they rarely call because you will tell them of your problems. I used to get my social support from my family but all is gone. I live in isolation only my neighbor tries to help me once in a while. Everything is a struggle I never stop to think and worry that if I died now my loved ones will not even be allowed to send me off decently. It is a terrible time and the worst moment of my life. Please keep communicating to me it’s very reassuring to hear from people like you, you care. May God bless you and your team, I am now part of the palliative care family…”
Vicky’s (Peace Hospice Adjumani) motor bike riding skills have been so handy during this period as she is able to ride and get to her patients and be able to offer care and support.
Vicky says “……Amidst this pandemic we need to hear a voice that gives hope and care, this was made possible by the airtime! My physical presence with the patients in the community hasn’t only improved the quality of their life but it brought unity and peace in people’s homes because the pain is gone. Today those referrals made directly to Lacor or Mulago near pass via the Palliative Care Unit, friends even amidst challenges there is something for us to learn, lets trace it….. “ Vicky
My motivation comes from the smiles of Hope of my patients!
Toko Friday is our volunteer coordinator and he directly supports palliative care patients as part of the multi-disciplinary team, during this period he has continued to bring joy and hope to the patients and families, he provides psychosocial, spiritual assessments and support, helps patients navigate complex networks, refers patients to other services and offers practical support such as accessing medications and physical exercises.
However, during this period due to the government’s measure of a ban on public and private transport getting to the hospital he has to walk 18.6kms to Mulago and back in order to offer support to patients with palliative care needs and along the way he encounters different police checks and being a rainy season sometimes the heavy rains hinder him as he walks but because of the love and passion he has for the vulnerable patients he endures all this so he is able to continue offering the help and support even during these difficult times and moments and his motivation comes from seeing his patients smile with hope as they appreciate his care and support.
Connecting!
Being able to access internet during this lockdown has made a huge different and enhanced our interactions with other palliative care providers locally and internationally as we are able to join various discussions on issues emerging as a result of Covid-19 and the impact on palliative services, we have been part of these, learnt and shared.
Locally the Palliative care Association of Uganda (PCAU) has organized zoom meetings for the palliative care fraternity in Uganda, these are weekly discussions and are ongoing. Some of the topics we have discussed have included;
- Psychosocial support for people affected by the COVID-19 pandemic
- Cancer services in Uganda during Covid-19 – response.
- On International Labour Day; recognizing and honoring all palliative care providers that have contributed to the growth of this specialty in Uganda.
- The right to Palliative care Uganda, during the Covid-19 pandemic outbreak
The aim of these discussions to remain updated on what is happening, challenges, suggestions and support solutions to the Covid-19 pandemic.
The African Palliative Care Association also organized a discussion on; Strategies to engage African communities to be proactive in the prevention of COVID and we were happy to be part of it.
ICMDA webinar: Palliative care of Covid-19 patients in low resource settings by Dr. Mhoira Leng
These are just some of the sessions that we have participated in but they are so many and we have learnt a lot and continue to learn.
Self-protection!
Our team is dedicated to providing the care and support to the patient and their families but they also need to feel protected and now that we got the equipment, we will do our best.
“We expect to offer good health for everyone and a comforting and dignified death for those departing” Florence
We thank you for your continued support.
God bless you all and please stay safe!
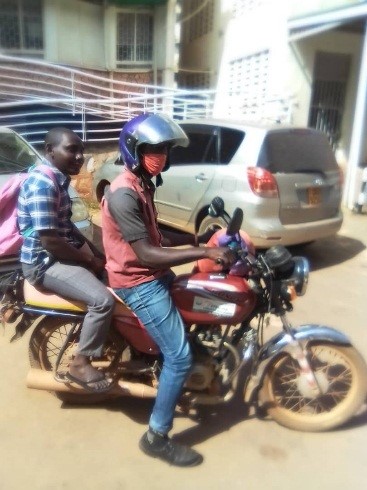
Ronald on his way to the Cancer Institute to receive his radiotherapy treatment

Vicki and her motorbike getting out to her patients

Toko walking to work

“We expect to offer good health for everyone and a comforting and dignified death for those departing” Florence
Humanity until infinity: life and hope in the times of COVID19
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 2nd April 2020
2nd April 2020
As I write this I am acutely aware the world has changed almost beyond recognition on the past few weeks. A pandemic much discussed in theory by the scientific world and the subject of movies has been unleashed by means of a tiny virus that has closed countries, pressed paused on economies, placed almost one third our world’s population into lock down. This outbreak has led to the deaths of tens of thousands…a number which is yet to rise.
In Uganda where I am also self-isolating and in lockdown I reflect that this country and its neighbours are well used to infectious disease. Malaria, HIV, TB and Ebola are well known here. Let me share a few statistics from 2018 that of course represents real people and real challenges. 37.9 million people were living with HIV and 770,000 died from HIV/AIDS. TB affected 10m worldwide with 1.5 million deaths of which 205,000 were children. Malaria, the often forgotten scourge in tropical climes, affected 229 million with 405,000 deaths and 67% of these were children.
COVID19 is affecting people accross ouir world….an infectious illness affecting people from all walks of life and all parts of the globe. This is a global humanitarian challenge with as ever those on the margins most affected. Money, position, power does not protect us and in many ways this demonstrated more than ever our shared humanity. It is also highlighting our common sense of helplessness. In low income settings the impact of COVID19 is deeply felt where there are no margins of resources. People who rely on a daily wage to provide food for families are struggling accross Africa. Transport blockades have affected migrant workers causing huge shifts of population in places like India. Struggling health systems in high income countries are well documented and the effect on poorly resourced health systems is only becoming clear for patients and families with many different health problems. Add to this refugee setting such as our partners in Northern Uganda working with South Sudanese refugees and in Gaza where they have already endured 11 years of siege and restrictions….can you imagine! We need to advocate for the ending of barriers, blocades and sanctions that are putting people are a greater risk than ever.
Let me tell you about Ronald, one of our most dedicated and loyal volunteers in the palliative care team in PcERC in Kampala. He was diagnosed with cancer just a few weeks before he married his sweetheart Christine at the end of last year. We have been raising funds and supporting them as he completed surgery and chemotherapy but now how does he access his radiotherapy? There is no public transport, private car costs more than a day’s salary but today even that is not permitted, so he is borrowing a bicycle for the 45 minute trip each day… not an easy feat when you are unwell. Yet, he still says ‘Many thanks for all the support….MMPCU has been like a family to me’.
Dr Peace Bagasha is a palliative care and renal medicine consultant in our team, and she told me about her journey to work yesterday. ‘I was stopped 10 times by police road blocks trying to get to the renal dialysis unit. Most of the nurses are unable to attend to patients as they live on the edges of the city due to housing costs and low wages and are now struggling to get to work. We are hopeful that stickers to permit essential travel will be made available soon.’
Vicky Opia, lead palliative care nurse in Adjumnai Hospital where a COVID19 positive patient has been admitted tells me: ‘People are afraid. Can you imagine, a nurse riding a boda to work in her nurses uniform was beaten?’
Where is the hope and where is the humanity at a time such as this? I think is it right in front of us, within us and amongst us. All over the world we see how compassion and courage and kindness are lifting spirits and making unique contributions. We see a shared common experience and greater empathy for our global community and standing together. Creativity for scientists, technology experts, health care workers and families has never been higher. We are thinking about what really matters, what is the focus and source of our hope. Many are looking outwards to how we can help and encourage each other. Many are thinking about our enviromnmnet and realising our interconnectedness with the health of our planet. Many are growing spiritually and faith in God. Candles stand in windows and rainbows colour our lives.
In palliative care this language of open communication even about the tough times in life is very familiar. We hold that place of uncertainty with those facing life threatening and limiting illness. We seek to listen, show compassion, offer skilled holistic help, journey with people through the dark times and the bright times, reveal and redirect hope and support people to build resilience.
I have been moved by this meditation from William Brodrick...'We have to be candles, burning between hope and despair, faith and doubt, life and death, all the opposites. This is the disquieting place where people must always find us. And if our life means anything, if what we are goes beyoind the walls and does some good, it is that somehow, by being here, at peace, we help the world cope with what it vcannot understand'
We are working closely with our partners who areare busy developing guidelines, working out how to work through non face-to-face means, doing direct patient care and advocating for effective PPEs and showing what amazing contributions health care workers and social and pastoral support workers can achieve. CairdeasIPCT is seeking to offer more financial support and if you feel you can partner with us many thanks. You can donate here. We are seeking to address the anxiety and fear with our partner Prof Chitra Venkateswaran, a psychiatry specialist in India, leading ways to train and support families using virtual means.
Let this be a time of standing together, talking to each other, listening, sharing our common humanity, caring for our neighbour, the stranger, the vulnerable and marginalised, the broken and fearful in our communities local and global. Let this be a time for all walls and differenecs to crumble and be brought down. Let us move forward with renewed hope, deeper joy and fresh purpose.
Useful resources can also be found at www.thewhpca.org/covid-19

Bringing hope
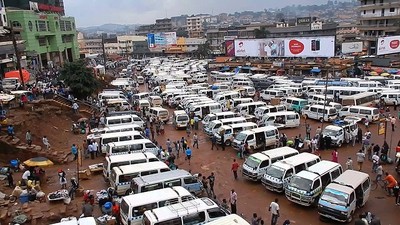
Kampala taxi park before lockdown

Kampala taxi park after lockdown

Palestinian artists Samah Said and Dorgham Krakeh paint N95 respirators for a project raising awareness about Covid-19 in Gaza city


Sanyu support team

Providing palliative care for host and refugee communities in Northern Uganda
![]() Ian Robinson
Ian Robinson
![]() 31st March 2020
31st March 2020
Godfrey knew he wanted to become a nurse when his father became sick and he didn’t know how to care for him. Living in Adjumani district in Northern Uganda, Godfrey studied to be a nurse. His favourite part of the job was speaking to the patients, particularly those with chronic illness. These patients seemed to have a different perspective on life; a unique sort of peace. He took part in a palliative care leadership course in the district facilitated by Cairdeas. Godfrey now volunteers for Cairdeas partner, Peace Hospice Adjumani. Peace Hospice works to provide palliative care services in the refugee settlements and to host populations.
I met Godfrey on a recent trip to Uganda. As Operations Director of Cairdeas I had the opportunity to visit Uganda to meet partners, visit patients and gain a deeper understanding of how the work of Cairdeas is empowering communities to provide palliative care to those in need.
I accompanied Godfrey to a home visit in Adjumani in Northern Uganda. Esther (name has been changed) was suffering from advanced cervical cancer. She was being looked after by her sisters and visited by the Peace Hospice team every two weeks. Esther was on high doses of morphine to manage the pain but was still experiencing some symptoms and side effects of the morphine. Godfrey gave Esther some advice on managing these symptoms, such as waiting an hour after taking the morphine and before eating to avoid nausea. As well as enquiring about her medication and symptoms, Godfrey checked in on the care Esther was receiving from her family and how she was feeling emotionally and spiritually. She explained that she was being cared for by her family, but also that she knew she wouldn’t have to feel the stress of loneliness because the hospice team will take care of her. Before we left Esther took the opportunity to practice her English with me. “At least I have laughed for today” she said to Godfrey in Madi as we left.
We then went onto the first refugee settlement, Pagirinya. Village Health Teams (VHTs) have been trained to identify patients with palliative needs and refer them to the Peace Hospice team. Godfrey and I waited under the shade of a tree as the VHT went to find the patient we were there to see. As we sat there, I was struck by how well established the settlement was.
Uganda has welcomed around 1.3 million refugees – the third largest refugee population in the world. A recent episode of the BBC documentary, The Displaced, followed Ashley John-Baptiste as he met some of the refugees settling in Northern Uganda. “Instead of fighting the tide of displacement, Uganda has become renowned for its welcoming refugee policies”. The settlements I saw weren’t dissimilar to the host villages – mud hut homes, vegetable patches, clothes hanging out to dry, goats and other animals running about. When being forced to leave one’s home, those crossing the border into Uganda are welcomed with a dignified space to set up camp until it is safe to return home.
The first patient we saw was a man with painful swelling in his legs. The swelling had started in his left leg and spread to the right. He was receiving pain killers from the Health Centre which is run by UNHCR – the United Nations refugee agency. He had been offered a biopsy but couldn’t afford the cost of the results. He didn’t feel he was getting any support from the community. “You are not alone, we are here for you” Godfrey assured him. The patient may be transferred to a hospital in the nearest city, but the Peace Hospice team will ensure he doesn’t slip under the radar and will support him in whatever way they can. Finance is often one of the biggest challenges in these situations, and unfortunately Peace Hospice itself struggles with this. As a key partner, Cairdeas hopes to be able to support them through joint funded projects.
The second patient, Pal, was a lady with advanced rheumatoid arthritis. Pal couldn’t stand without support from her daughter. She had recently been walking with a stick, but the stick had broken, causing her to fall and break her hip. Godfrey promised to help the family by sourcing a stretcher or wheelchair to make it easier to move their mother around. He prescribed some medication and wrote a note to the nearby health centre asking them to provide further support for Pal. “I will not forget mama, I will not leave her” Godfrey reassured Pal’s children.
It was an eye-opening experience visiting both the Adjumani host communities and the refugee settlements. I was given an insight into how a country can successfully welcome people who have had to flee their home countries, offering refuge and dignity in their displacement. It was wonderful to see the work of Peace Hospice and the support they are offering to those in need. They were able to offer assurance that the patients would not be left to suffer, treating their symptoms and seeking further health care from the relevant organisations. Godfrey gave each patient time and space to share their worries, making them feel cared for and valued as an individual.
Please remember Peace Hospice as they face the Covid-19 crisis. Adjumani hospital where they are based has confirmed a first case of the virus and, as yet, there is no evidence of it spreading to the refugee settlements. Executive Director of Peace Hospice and key Cairdeas partner, Vicky Opia has been appointed as the lead for psychosocial care at Adjumani Hospital. Our thoughts and prayers go out to Vicky, Godfrey, and all those working to care for both host and refugee populations in Adjumani at this time.

Godfrey with our first patient, Esther

Godfrey with VHT, Madig Madig
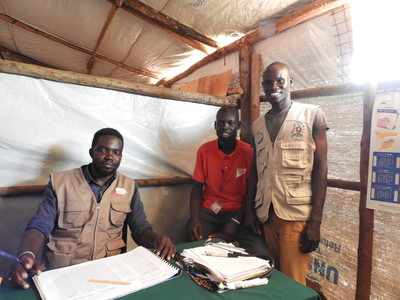
Godfrey with VHTs and Healthcare workers in the refugee camp
