
BlogBe notified of new blogs
Upcoming Event February 7th: Palliative Care: Rethinking Coping, Exploring Hope, In the Midst of Conflict and Change
![]() Cameron Don
Cameron Don
![]() 16th January 2026
16th January 2026
Hello friends and supporters, and happy New Year! We hope this year brings peace and joy to you all. As we look forward at the Cairdeas plans for this year, we want to share with you an exciting event coming up which we are looking forward to, and hope to see many of you there.
On February 7th, we will be co-hosting a palliative care conference, in partnership with Edinburgh University’s Global Health Academy & PallCHASE, in George Square, Edinburgh. Entitled ‘Palliative Care: Rethinking Coping, Exploring Hope, In the Midst of Conflict and Change’, the conference will focus on palliative care in fragile settings affected by conflict, and the support needed by patients and healthcare workers in these settings.
With humanitarian crises ongoing in Gaza and Sudan, this conference is a timely event speaking to vitally important issues. Over the past few years we have seen healthcare workers targeted in these and other regions, and it is critical that we are equipped to support them, so that they can continue to support their extremely marginalized patients.
The conference is host to an exciting line up of speakers, bringing expert knowledge and perspectives from all around the world. Featuring presentations by Rev. Rick Bauer, Dr. Nahla Gafer, Dr. Yasser Abu Jamieh & our own Medical Director, Dr. Mhoira Leng, we will hear perspectives from USA, Sudan, Gaza and Scotland.
As the rapidly changing geopolitical landscape continues to affect how countries co-exist and how responses to humanitarian emergencies are coordinated, having such a breadth of global perspectives makes this an invaluable opportunity to learn more about palliative care around the world.
Tickets are still available, and you can register now for this exciting event by clicking here! We also ask you to consider sharing with friends and colleagues who may be interested.
We look forward to seeing you in Edinburgh on February 7th!
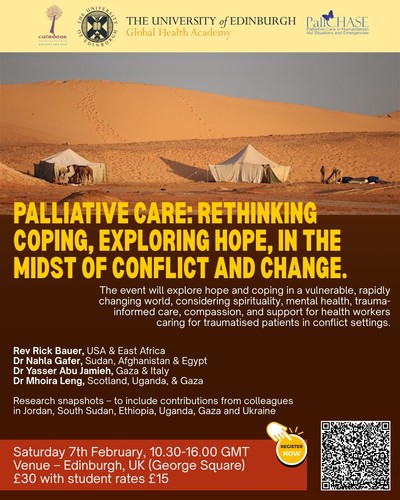
Conference Poster

Dr Nahla Gafer & Dr Mhoira Leng, two of our speakers
Cairdeas Christmas Message 2025
![]() Cameron Don
Cameron Don
![]() 19th December 2025
19th December 2025
As I stood in Manger Square in Bethlehem amidst the sparkle of the Christmas tree being lit, there was a palpable sense of joy, yet tempered by sorrow.
For 2 years the celebrations of Christmas have been cancelled…though of course not Christmas itself. The words of Maher Canawati, the Mayor of Bethlehem, a city twinned with Glasgow, spoke clearly;
‘As Bethlehem lights its Christmas tree, the deep anguish endured by our people in Gaza does not leave our hearts. The wound of Gaza is our wound, the people of Gaza are our people, and the light of Christmas has no meaning unless it first touches the hearts of the afflicted and the oppressed all over Palestine….Through these celebrations, Palestinians send a message of resilience – to say we are still here, determined to live, to keep Bethlehem the capital of Christmas, and to continue telling its story. Palestinians love life.”
His words speak into the deep meaning of Christmas. A time where there is joy, hope and love shared by us all because of the birth of a Saviour in Bethlehem, who was announced with great joy and great promise. They also speak of a deep longing in the land of the first Christmas for peace, for justice, for global solidarity and support from a people who show great courage and steadfastness. The word ‘sumud’ sums up this courage.
For many of us this time of year brings so much joy yet for others it is tinged with sadness as we remember loss, experience loneliness and long for hope, love, peace and reconciliation to be seen in our families, our communities, our nations and our world.
Palliative care has at its heart humanity; the recognition of each person being precious and unique and deserving of dignity, support and access to healthcare in their time of need. Our Cairdeas gathering recently showcased humanity and dignity as partners shared their work but also the values that underpin all they do and are. If you missed this encouraging event the videos are available on our website and will be shared on our social media pages soon. We pay tribute to all our incredible colleagues and partners in Uganda, Palestine, Sudan and India who show this humanity and offer dignified care in so many places and to so many people even in the most challenging of circumstances. We thank our supporters and commit once again to use whatever resources are given to us to work together with our partners for a world where palliative care is available to all in need.
More than ever this year we welcome financial support as a generous legacy from one of our original supporters will be nearing an end in 2026. Read below about our renewed fundraising efforts for 2026, and our February global palliative care conference.
Many of us will sing the carol O Little Town of Bethlehem this year, with the poignant words ‘Yet in thy dark streets shineth an everlasting light. The hope and fears of all the years are met in Thee tonight. O come to us, abide with us, our Lord Emmanuel! ’
As we celebrate in our different ways this Christmas, and at the end of 2025 with all its joys and sorrows, we also look forward to 2026 with hope. This hope is not mere wishful thinking but is both a deep reassurance and a call to action. I share a beautiful poem written by a Palestinian poet, Khawla Badwan.
‘There is no hope, be the action that restores hope
There is no justice, be the voice that speaks of justice
There is no courage, be the witness that lives in courage.
There is no light, be the holder that forces light
There is no mercy, be the heart that teaches mercy.
There is no language, be the crafter that makes language.’
Wishing you and yours the blessing of joy, love and hope from the Prince of Peace this Christmas and every blessing for 2026.
Mhoira Leng
Medical Director
Upcoming in 2026
During the gathering, we shared some ways in which your donations go to making a difference in the lives of patients and carers in vulnerable communities. To help support the work of our partners and colleagues in crisis stricken places like Gaza and Sudan, please consider starting or increasing a regular donation, which you can do via our website, or through bank transfers: Sort Code 83-15-31, Account Number 11090398.
Looking to 2026, we are excited to be part-hosting a global palliative care conference on February 7th in partnership with Edinburgh University’s Global Health Academy and PallCHASE. Taking place in George Square, Edinburgh, the conference will explore palliative care in the midst of conflict and change and will feature talks from Rev. Rick Bauer, Dr Nahla Gafer, Dr Yasser Abu Jamieh and Dr Mhoira Leng. This will be an important time of sharing between colleagues, to register for the event and get tickets, click here.





Cairdeas Gathering 2025 & a Call for Support: Sunshine in War
![]() Cameron Don
Cameron Don
![]() 28th November 2025
28th November 2025
Hello to all of our Cairdeas supporters! As you may have seen, our 2025 Cairdeas Gathering is taking place soon, on November 29th from 3pm-5pm. It will be a hybrid meeting, so you can join us in person, at Kirkintilloch Baptist Church, or online by registering here.
In the run up to the Gathering, we wanted to share some ways that supporters can get involved and support some of the projects which will be discussed during this time. The past few years have been increasingly tough for charities and NGOs, as costs rise, donations fall and aid funding is drastically cut. Despite these challenges, we have continued to work to support our partners around the world as they deliver vital, compassionate care to patients and families, at times in the face of instability, targeted violence and displacement.
“Then we had the war. Without any warning, suddenly. Some people were trapped, some people were outside their homes and because of the war they stayed outside their homes for weeks.” Dr Nahla Gafer
One of the projects we support is the Sunshine in War project, working in Sudan to support patients and families displaced by the awful violence which has gripped the country during recent years. Targeted attacks on hospitals, skyrocketing costs of medical treatment and the difficulty and danger of travelling have all contributed to a difficult financial situation for the team. In the face of these enormous challenges, they have found innovative ways to continue caring for their patients, moving consultations online and visiting patients in spite of the danger to their safety.
“With the help of Cairdeas we managed to have an office in a city in the North…the team is working from the office there and connecting with other members and patients.” Dr Nahla Gafer
Cairdeas was recently able to facilitate a donation of around £4000 to the Sunshine in War team by PallCHASE, a close partner who focus on palliative care in areas of humanitarian crisis. Through this, the team have been able to continue using their office for administrative work, and their ledgers in Damar and Khartoum, providing a facility for patients to receive the physical, emotional, psychological and spiritual care they so desperately need. We are delighted that the team received this money, but with high costs and so many patients in need of care, we know that they need more.
“With these organisations supporting the team…we reached more than 800 of our patients and we are receiving new cases. They [the team] became known in the new places they re-located to.” Dr Nahla Gafer
We want to increase the support we give to the Sunshine in War team, and we can only do that through donations from our supporters. If you are able, we would like to ask that you consider setting up a regular donation, to allow us to support this amazing team doing such critical work for some of the world’s most vulnerable people.
If you are already a regular donor, we thank you for your support, and ask if you would consider increasing your donation amount, to allow us to increase the support we can give to Sunshine in War, during a time when the violence in Sudan is at a frightening level, and people with life-limiting illnesses are extremely vulnerable.
How your support makes a difference:
- £10 funds 5 patients’ virtual care for a month
- £20 funds 4 in-person patient visits by the team
How to Give:
- Click here to go to our donations page – choose Sunshine in War in the dropdown menu
Thank you, from all the team at Cairdeas.

Palliative care team in purple for world palliative care day. Dr Nahla Gafer, Cairdeas Sudan lead pictured (2nd fromright)

Nurses on a patient visit

Sudan palliative care team with Dr Mhoira

The team with a patient
