
#BuildingAWorldThatCares with Cairdeas
![]() Lakshmy Venkatesh
Lakshmy Venkatesh
![]() 3rd December 2021
3rd December 2021
Hello all! For the past two years, the world has been struggling with COVID-19 and other kinds of strife and challenges. While the work of Cairdeas has been continuing despite restrictions and COVID-19 lockdowns, our supporters continue to be the pillars of our work. Our supporters provide us the ability to intervene in areas and geographies which remain unaddressed or partially addressed. We seek support not only in the form of funds but also in terms of time and skills. Through this blog, we at Cairdeas hope to inform our supporters of some of the different ways to get involved with our work and the immediate requirements on our end.
Donations
There are several aspects of Cairdeas' work that you can support by making donations. We work with partners to ensure people living with serious chronic illness have access to the help they need and deserve; help that improves their quality of life, helps with pain and other symptoms but also supports them in other ways such as worry, hope, choices, goals and dignity. This is what we call holistic palliative care and Cairdeas seeks to listen to the needs of people and build up services and train people to be leaders for this care in their own setting. We work to influence policy, develop training programmes, build teams, empower communities, mentor leaders and so offer high quality, evidenced based palliative care to the most vulnerable and marginalised. In this context, Cairdeas’ interventions grow permanent sustainable palliative care services by the careful cultivation of local capacities through:
Trainings (building capacity of village health teams and healthcare workers to provide palliative care support in humaitarian contexts)
Scholarships (ranges from a day or week long course through to the 1 year diploma and 3 year degree programmes in palliative care at Makerere University and Mulago Hospital in Kampala with Hospice Africa Uganda)
Capital Expenditure (bicycles, transport, tech support and t-shirts for volunteers)
You can find details of how to donate to specific appeals or to set up a one-off or regular donation to the work of Cairdeas here.
Work with us
Through Cairdeas, you gain the opportunity to be a changemaker. We are looking for people who are passionate about helping those with life limiting illness and people forced to grapple with such conditions in under-resourced contexts. Are you one of those people? If you are, then Cairdeas offers you the opportunity to:
Join our board (Do you have skills in finance, fundraising and communications? The trustees are looking to strengthen their board with those who have skills in finance, fundraising and communications to support the work of Cairdeas. If you are interested or wish to discuss any involvement please contact Andy Smith our Chairman at chair@cairdeas.co.uk. Join a work culture that empowers every stakeholder to share ideas and take responsibility.)
Volunteer your time (Do you wish to engage in exciting work, often in challenging contexts? At Cairdeas, we aim to think outside the box. We encourage ideas and give responsibility to all supporters at all levels, to help solve the complex issues that we face. You will have many opportunities to be heard and take the initiative. We require support especially in the areas of communications, fundraising and digital engagement with our donors. If you think this is for you, please fill in the form by following this link.)
Get an internship (In the field, we work hard to solve challenges in demanding environments, often in hard-to-reach areas. We work professionally, with respect for all and focus on safety and teamwork. You will learn fast in a professional setting. We require support especially in the areas of communications, fundraising and digital engagement with our donors. If you think this is for you, please fill in the form by following this link.)
We rely on the generosity of supporters for us to in turn provide support to those in need of palliative care and palliative care training and so we also request all our supporters to share this information widely, with all those who might be interested in engaging with Cairdeas IPCT. Let’s build a world that cares together!

#BuildingAWorldThatCares
Palliative Care Training at Gaza through Cairdeas Partners, by Elizabeth Swain
![]() Cairdeas
Cairdeas
![]() 26th November 2021
26th November 2021
Imagine you are Maram. You are a 20-year-old young lady and have just started your clinical training at the Islamic University in Gaza. You live with your parents and have been relying on your mobile phone for taking part in training sessions.
___________________________________________________________________________________________________________________
Day 1
Will the internet be good enough for me to hear what is said?
Will I understand the English of the teachers from outside Gaza and what if I have to answer in English? Someone told me that the teachers are from about 4 different countries and of course we have our own teacher Dr Khamis – we all like him a lot.
…and anyway - what is this subject “palliative care” we are to be taught – I think it is something to do with dying and I have seen and heard so much of this while we had the bombing and do not really want to be reminded of it.
Day 2
Well, the teachers form outside Gaza are a bit strange but seem kind and most of them are speaking slowly enough so amazingly I can understand most of what they say.
We discussed a business man who has cancer and whose son is going to go away to study – this made my classmate Doaa very sad as she has an uncle that this happened to – he did not want his son to miss the opportunity to study but he never saw him again as the authorities would not allow him to enter Gaza when he was dying. She phoned me after we finished and we both cried.
Day 3
We have had a session about controlling pain. This is all new to me as we have not been to the hospital yet. However, I did understand a lot of what the Dr said as my grandmother has bad pains sometimes and only takes her painkillers if the pain is very, very bad. I learnt through the session I can now suggest that she takes it regularly. I feel sure now that this will help her. I will try and explain about taking tablets and not injection.
At first when I was asked to play the patient in a little play we did, I was not keen, but I actually enjoyed it! Although it was a sad story, I realized that knowing what was wrong with me – even if it is something bad – was in the end a good thing. Knowing meant that I could talk to my family about it. I like it when people tell me the truth.
Day 4
I am beginning to understand more and am really pleased I can do this course. For me it is more interesting than sitting in a classroom and having a professor talk at us for an hour with no questions. And I really like discussing things. Some of the other girls in my group cannot talk to the teachers because their internet is not strong enough. I felt bad for them because I know they want to be able to ask questions. Ola gave me a question to ask and the doctor who did our group session tried really hard to answer. It was about was how our religion says that to suffer pain makes us better Muslims. It seemed to me it was not really a question that Ola wanted to know the answer to.
Day 5
We all thought we would have an exam today but no we don’t! I think I would do okay because I have learned a lot and it is not so difficult.
The session today was about caring for ourselves. It seems a strange thing for us to study as we are going to be doctors; we are to look after other people. But I could see towards the end of the session that if I get something called burn-out then I cannot help other people. Each of the teachers gave us an idea and this was interesting – they seem to be just like us.
They said they would like to come and visit us next spring so we can see patients with them. I really, really hope they come. We talked about all sorts of things with them and I want them to try Gaza food.
___________________________________________________________________________________________________________________
Thank you Maram – it was good to meet you and your class. We, alongside Dr Khamis Elessi the IUG lead for palliative care, were all very impressed by your hard work and willingness to engage with us although we know some of you really struggled with the internet connections. We, too, hope to be able to come in April and meet some of you in the hospital wards and would try to find ways of catching up with the clinical case teaching.
The feedback that we had from you all encouraged us and here are some samples:
“I learnt how to communicate well with patients and their relatives and the difference between empathy and sympathy. and another important thing is how to relieve the pressure inside me.“
“I have learned about thinking of the patient’s situation from all aspects, and how we can practice ourself more to understand their psychological, social and spiritual pain.”
“I have learned to care and treat the patient as a whole person and not only physically because some patients need to treat the spiritual side for example more than physical side.”
“I also learned that we may reach the situation that there is no point in any medical intervention for the patient, but there is an important aspect that we can still do, which is palliative medicine.”
“I learned to treat patients as humans not as a problem to solve, and that I am as a doctor have feelings that I need to respect and accept."
“Remember that patients are human, and do not forget that yourself are human too.”
Some one took a screen shot of the feedback session – we had asked the question about what values you saw being demonstrated in Palliative Care.
I do hope that this gives you a flavour of our Gaza teaching. This is the second year we have had to rely on online teaching and you will have seen some of the challenges for all involved. We taught students just beginning their clinical studies – a good time we felt to expose them to the concepts of whole person medicine and palliative care.
Each day we started with a mini lecture for half of the class (we divided the year group of about 150 students into boys and girls as is customary in the Islamic context). The group then went into breakout rooms in groups of about 12 for case discussions around 6 different patient scenarios.
On our next visit in, hopefully in April, we will focus on building the clinical services and linkages and exploring ways to support a new comprehensive cancer centre alongside our partnership with IUG.
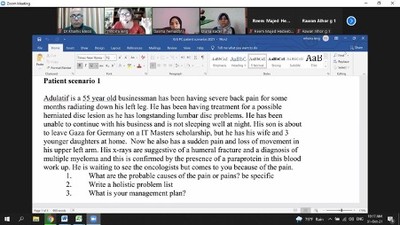
Session in progress
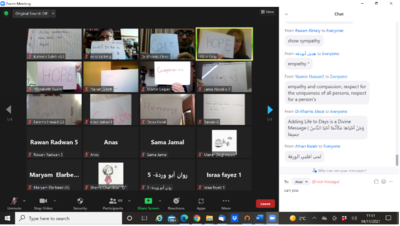
Responses to what palliative means to the students
Integration of palliative care into healthcare provision for South Sudanese refugees and host communities in Adjumani and Obongi districts of Uganda, By Elizabeth Nabirye
![]() Cairdeas
Cairdeas
![]() 3rd November 2021
3rd November 2021
Empowering communities and health systems to address health related suffering in host and humanitarian settings through capacity building and integration funded by UKAID.
Background
Palliative care (PC) is rarely prioritised or integrated in humanitarian settings and so evidence is needed from field settings to inform integration of PC in health systems. Uganda is the 3rd largest host for refugees globally, and previous work with Ministry of Health of Uganda (MOH), Peace Hospice Adjumani (PEACHOA), Palliative Care Education and Research Consortium (PcERC) and Cairdeas (IPCT) to integrate PC in Adjumani district, with a population of 210,000 refugees, 240,000 hosts) included training of Village Health Teams (VHTs) and Healthcare Workers (HCWs). This is now being extended to the new Obongi district with a population of 120,000 refugees and 50,000 hosts.
Rapid Systems Appraisal (RSA):
A RSA was conducted with the aim to evaluate the setting and systems affecting chronic diseases and health related suffering for refugees and host populations in both Adjumani and Obongi districts.
The methods:
This included documentary review, mapping of key stakeholders, observing of practice, qualitative interviews with 4 groups of informants: patients and their caregivers, palliative care providers, key opinion leaders; MOH, humanitarian stakeholders, community and healthcare workers.
The broad themes following thematic coding and analysis of 40 interviews included
- Health system issues; planning, resources, capacity, pathways of care, integration
- Understanding of palliative care
- Education and training
- Impact of palliative care
- Challenges and gaps
- Community and HCW experience
- Culture and stigma
Results:
Health system issues; these included issues relating to planning, resources, capacity building, pathways of care, integration
“There are a few things that can make you be able to integrate palliative care; One is ownership...it is not a peace hospice project but an Obongi district government programme. Ownership goes with leadership... the members for health need to take the leadership.” Hon Dr. MP
“At community level it is only one person and this remains a challenge. …plan for the future of palliative care strategically… so that there is no gap in patients care” UNHCR
“At the Humanitarian aspect, the time of making proposals to the funders on what they are going to implement, the picture is of comprehensive health care, which is always sent out but palliative care may not come out pronounced and there is need to have that strong advocacy of this component. There is time for all this to change through advocacy and training” Dr MTI
Understanding of palliative care and planning
"I thought palliative care was last office. Where there is nothing we can do and we just care for them, as they wait for their own death and I never thought this would need any technical person." Health worker
"Palliative care is like manna from heaven’ ‘I pledge to include it in district strategic planning’" RDC
"Palliative care is very important...it has touched my heart…this programme is the best investment for so far because it prepares the heart of the people ...we are answerable in future, when I was sick and bedridden you gave me care....’" Community leader
"There are so many people in the community with chronic illness but by the time we discover them, it is too late so we need to create awareness and also embrace palliative care’" DHO
Education and training
“One of the challenges is the skilled staff to give the services, a few staff who have been trained and even commitment is a challenge
Doing capacity building training is very important....training and skilling primary and secondary care ...but also include leaders so they know what is being implemented.” Health worker
"VHTs, they are really so useful in the community because they can identify any condition, report and refer. So building the capacity of the VHTs is very important, and the component of research is equally very good, it gives evidence.’"Health care leader
Community experience
"We need to work together and be on radio to share. People can be abandoned mostly because of ignorance...people think someone who is sick can infect them...such as cancer. This programme is the best investment, so far because it prepares the heart of the people’"Community leader
"But our communities here thinks that when someone is very sick, they should be cared for in the hospital and die from hospital, so taking them home is considered to be a taboo’" Health care leader
"We thank our Almighty God to have given heart to the people of this organisation to come and us...this is God’s love to our district...without God’s love they would not come this way’" Faith leader
Impact of Palliative care
"So whenever I pay a visit, it’s like am bringing glory to their home. We really smile, we really laugh so whenever we are in that community, they are really appreciating our service and always tell us that without us, they would have not lived up to this time. That is encouraging. So they are really pleasing me so much, I bring hope to them, but when I lose one, I’ve also lost hope too.’" PC worker
Challenges and gaps
"Facilities don’t have morphine and other drugs but also health workers need to be trained to be able to assess these patients and manage their symptoms." Health worker at health centre III
"Because I lack the knowledge, I just don’t even attend to them, I just refer them to other Health care workers As health workers we sometimes do little to help these patients with chronic illness, for example at times their symptoms are so complex that we can’t manage them because of knowledge gap." Health worker at health centre II
"These patients have a lot of symptom burden especially pain which is always uncontrolled with available pain killer that we give them. Available pain killers include Paracetamol and diclofenac at times ibuprofen. We don’t have morphine at our facility. " Medical Clinical Officer
Culture and stigma
"But our communities here thinks that when someone is very sick, they should be cared for in the hospital and die from hospital, so taking them home is considered to be a taboo that is the other challenge " Doctor
"When they have chronic illness they can’t support themselves, but also the refugees have different cultures and this can be a problem taking care of them, some use their local herbs." Nurse
Conclusions:
PC service integration is needed and previous interventions were effective but we need to extend to all aspects of planning and implementation.
Refugee and host communities must have ownership and the services should be tailored to the community needs.
Further evidence on the PC needs will be collected including novel tools to understand community experience.
A comprehensive education package for HCW, VHTs and family caregivers and community mentors will be implemented and evaluated.
Acknowledgement
Many thanks to those who participated in this RSA which was led by Dr. Mhoira Leng, Elizabeth Nabirye, Vicky Opia, Godfrey Oiti and the entire PEACHOA team. Special thanks to all our participants (patients and families, VHTs, Health works, opinion leader) and funders.

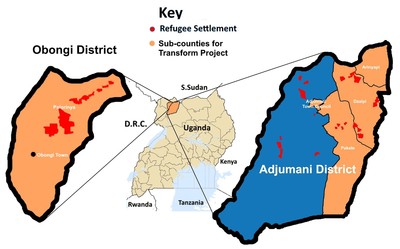
Setting of Obongi district

During an observation visit of a palliative care health worker with a patient

Interview with people (VHT) who interact with patients with chronic illness

Leaders of the programme across the Nile
