
The Religions of the World Charter for Children’s Palliative Care; a ground breaking initiative.
![]() Cairdeas
Cairdeas
![]() 11th March 2017
11th March 2017
A few weeks ago Dr Elizabeth Swain, Trustee of Cairdeas and experienced palliative care and primary care clinician, was invited to attend an event at the Scottish Parliament and lend her signature to an important document highlighting the need for palliative care for children. She shares the experience and encourages us to sign up!
'There are a few hoops to jump before one can host an event at the Scottish parliament and one of them is to have the sponsorship of an MSP. EMMS (Edinburgh Medical Missions Society) had just that, with Andy Wightman MSP for Lothian giving his support. He gave this maybe for two main reasons –firstly EMMS is a very well respected Edinburgh based Christian organisation and this is their 175th anniversary year and secondly they are promoting the The Religions Of The World Charter For Children's Palliative Care which has been drawn up by the Maruzza Foundation, another well respected organisation based in Rome, which has the backing of Pope Francis.
So- hey presto, here we were in the Scottish Parliament on the evening of 8th February. I sat between the Moderator of the Church of Scotland and the Leader of the Mothers’ Union and just in front was a member of the Shia Muslim community. Silvia Lefebvre D’Ovidio, a Trustee of the Maruzza Foundation, was there is person to present the charter. This is a universal declaration by all faiths that children's palliative care provides the best solutions for all children and young people affected by life-threatening and life-limiting disease and, further, that access to palliative care services should be a right.
The Religions of the World Charter for Children's Palliative Care is a ground breaking initiative. Its purpose is to dismantle the barriers which prevent over 20 million children worldwide affected by serious life-limiting illnesses from receiving care that is appropriate to their age and disease. Religions have global reach and, due to their broadly-recognized moral authority, can provide fundamental support for children's palliative care provisions by:
affirming that all children with serious illness should have guaranteed access to palliative care
confirming that alleviating pain is a moral and religious obligation
recommending to political leaders and policy makers that children's palliative care should be integrated into every national healthcare system
giving strength to the movement for the global availability of children's palliative care through the involvement and endorsements of all religious, faith, and community leaders.
The Charter was first drafted at the Vatican by representatives of the main world’s religions, leading paediatric palliative care specialists, human rights experts and young patients and their families. Scotland, with its global reputation as a leader in palliative care advocacy, now has the opportunity to get behind this Charter and speak up for the 20 million children across the world affected by life- limiting illness. It is imperative that all these children and their families are guaranteed the right to access appropriate care that encompasses emotional and spiritual support.
After several moving and helpful presentations the delegates signed the charter in hard copy but also on line and you too can do this. Follow this link http://religionsworldcharter.maruzza.org'
Thanks Elizabeth for representing us and to EMMS for organising this important event.
If you want to read more about EMMS work please look at their website; you might also have seen tweiir ffanstiics films form Nepal in STV. Ihttp://www.emms.org/about-emms/the-news/stv-in-nepal/ ITo find out more about palliative care needs in children worlwide please look at the International Children's Palliative Care Network website http://www.icpcn.org/ which is now chaired by Prof Julia Downing and doing such a great job internationally.

Scottish parliament building
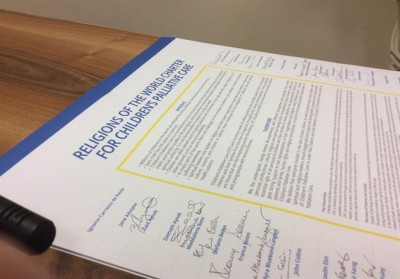
Charter and original signatures
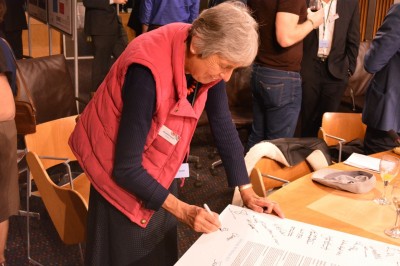
Dr Elizabeth Swain signing on behalf of CairdeasIPCT

Andy Wightman, MSP, signs charter
Hidden lives, hidden patients; refugees
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 24th February 2017
24th February 2017
Hidden lives and hidden patients was the title of an excellent session at the recent IAPCON 2017. (see presentation 'Refugees' in resources section 'IAPCON 2017') I want to reflect a little on palliative care in one of the most vulnerable populations..... those affected and living in the midst of complex humanitarian situations. These includes natural disasters such as the 2014-2016 ebola epidemic in West Africa or the 2016 earthquake in Nepal where I am currently visiting but also the huge needs of those affected by conflict.
In these complex situations the rural areas are often most affected where health care is already a challenge. In addition the understandable focus on urgent care may mean that those living with chronic disease end of life care are overlooked and under resourced. More than at any previous time in history we are seeing huge movements of people forced, mainly because of conflict, to flee their homes. UNHCR estimates there are 65.3 million forcibly displaced people in our world with 21.3 million refugees, 10 million people who are stateless and only 107,100 re-setttled. While we hear so much about the numbers taking huge risks to get to Europe the majority of displaced persons stay in their core country or are hosted in nearby countries such as Turkey, Lebanon and Jordan. Uganda is experiencing a significant increase in refugees from South Sudan and I will write about this another time.
This is one of the major challenges of our age...how will we respond to this need? Will we be only focused on our own borders and back yard? Will we act as global citizens to defend rights, protect the vulnerable, offer shared compassion and be peacemakers?
Palliative care is one avenue for us to defend and protect this shared humanity. Let me share a little more about palliative care in one of the most complex and longstanding humanitarian situations..the Occupied Palestine Territories. The ongoing conflict and unresolved land issues result in huge inequalities, lack of access to basic necessities of living, lack of free movement and significant challenges with health care. A recent UN report describes this de-development and warns it might eb cecoem uninhabitable by 2020. In Gaza rising levels of chronic disease are accompanied by chronic stress and for many a sense of hopelessness. I have been privileged to visit Gaza on 2 occasions meeting amazing colleagues working to improve health care and in particular pain and palliative care. The recently formed palliative care steering group led by Dr Khamis Elessi has wide representation including WHO, academic institutions, UN , MOH and those delivering health services. They have identified some key priorities including education and training, access to essential medications. Policy needs and steps towards devoting rated service delivery and centres of teaching and excellence.UNRWA, the UN mandate, is seeking to address the need for chronic mental health within their family health teams. How do we approach palliative care when the overall needs seem so overwhelming and solutions few? One of the senior surgeons who has become world renowned for his surgical work in war conditions said 'our patients are in pain, we have no choice but to act'
The Islamic University of Gaza is seeking to integrate palliative care competencies into their curriculum and weclomed our partnership' starting with the undergraduate medical curriculum. (see presentation 'Gaza undergdaruate education' in resources section 'IAPCON 2017' ) Using international frameworks and our Palliative Care Curriculum Toolkit alongside the leadership from Dr Anwar Alshaihkalil, undergradute dean and Dr Fadel Naim, dean at IUG we worked with their innovative curriculum. Our international team (Drs Tony Jefferis, Janet Gillet, Colin Cooper and Mhoira Leng; from University of Edinburgh, PRIME, Cairdeas) agreed the core competency domains for palliative care and supported the first implementation. We met enthusiastic and interested teaching fellows and students who actively participated in the learning including role plays and group work...even walking up and down stairs breathing through a straw..to help understand how our patients feel. We spent time in clinical teaching rounds with patients and families from the medical, paediatric, oncology wards and intensive care. One memorable encounter was with a patient who was explaining his cancer diagnosis to the students but his son kept popping his head round the curtain to say 'dont say that dad you will be fine!'. A perfect scenario to model communication and the importance of including family members
Let me share some of the learning impact and give our Gazan students a voice....'the course added to the clinical practice makes us feel the suffering of patients and how we can help them’....'patients cope better when we tell them the truth' ....'I have learned to add smile and life to days not just days to life' ....thank you for ,....'I can do many serious works and have fun at the same time'....'we should never say there is never nothing we can do'......

IUG students

Mural by Banksy on dividing wall in Bethlehem

Ward rounds IUG

Teaching fellows and faculty

Class of 2016 palliative care

Beauty in the desert

Jerusalem prayer
Medicine for Investors
![]() Cairdeas
Cairdeas
![]() 11th December 2016
11th December 2016
It was a pleasure to have Jared and Bex Cordner working with us through Cairdeas in MPCU, Kampala. They contributed with expertise, skill but also willingness to learn, building relationship and embracing the challenges and joys of life in Uganda. Jared gives us a very interesting reflection from his business perpsective. Cairdeas can find it hard to share with you the need to build capacity rather then fundraise for more concrete projects so thanks to Jared for this very helpful view on our partnership with MPCU but also the fundamental principle by which Cairdeas seeks to work globally to increase acccess to palliative care for all.
'I’m not a medic. In fact that statement goes nowhere near far enough to explain my obscene lack of knowledge in relation to anything medical, despite being married to a Doctor (Bex). I come from a business background and so when Bex and I decided to take some time off from our normal jobs to travel to Uganda to work with Cairdeas I viewed the whole thing through different lens than she did.
Firstly, when I read that Cairdeas seeks to ‘promote and facilitate the provision of high quality palliative care in the developing world where such care is limited’, my finance brain summarised this as ‘making investments, not creating expenditure’. Working in an investment bank at the time I felt comfortable that I understood that world. Now, having almost finished our 4 months here in Kampala I find myself reflecting on the investment Cairdeas is making in Palliative Care in Uganda. I’ll summarise my thoughts using some standard investment appraisal techniques.
Capital Growth or Dividends
A central principal behind investing is that in repayment for your resources you seek either a dividend, or a growth in value. The investment that Cairdeas is making is focused on seeing growth, largely through capacity building within the palliative care teams across Uganda. I’ve seen that isn’t an easy process as it requires time, money, training and energy. All of these need to be utilised in developing appropriate skills in individuals, all of whom are different, as well as impacting practices. I believe that if we are to see true development in Uganda, then this is the approach which will deliver that.
Exit Strategy
Another key area that must be explored before you buy into any investment is that of the exit strategy, it is important to be able to walk away when the time is right. The capacity building approach which Cairdeas has adopted lends itself to a clear exit strategy as it increases self-sufficiency of the palliative care units across Uganda. It has been fascinating to observe how Mhoira has maximised the impact of Cairdeas, without fostering dependency. Personally, it has been a blessing to be able to offer whatever help I can, but my goal throughout was to ensure that I would never be needed again.
Ownership
Finally, there is a level of ownership and responsibility attached to investing. An investor should ask themselves, “Am I proud to be supporting these activities”? The work which Cairdeas is investing in is something to be exceptionally proud of. Cairdeas helps meets the deepest physical, spiritual and psychosocial needs of vulnerable patients in Uganda through its development of palliative care staff, volunteers and programmes. Basic human needs are being met in a way which they may not have been 8 years ago, and Cairdeas (through their local partnership with MPCU) are largely responsible for that.
So there you have it. In the past 4 months of being on the ground in Uganda I’ve witnessed Cairdeas make wise investments and ensure growth without dependency, all towards making palliative care accessible by all.'
Jared helped us put together our Christmas appeal so not too late to invest; it can be a practical breeding pig or enaging with our capacity building through scholarships or supporting our pastoral care and social support through our volunteer programme. Please use our donate button on the websoite and then drop us an email to say what you gave so we can keep you updated and send a photo! Lastly, do you have skills to contribute to Cairdeas vision either in the UK or in Uganda or one of the other places we work. Please get in touch and keep up with our news through this website and facebook!!

First time for Jared in the southern hemisphere

Thanksgiving at church; giving pregnant rabbits who are now multiplying!

Historic events as the Cranes get through to the Africa cup first time in ?60years

Bex and Jared as part of the MPCU football team at the PCAU tournament to celebrate World Hospice and Palliative Care Day

Enjoying the beauty and diversity of Uganda; the 'Pearl of Africa'
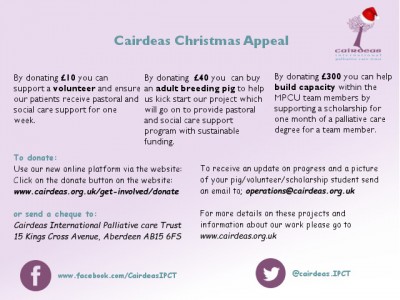
Still time to contribute; click on our donate button
