
Happy as pigs in muck
![]() Cairdeas
Cairdeas
![]() 6th September 2017
6th September 2017
It was great to have Dan (our operations director) and Felicity Knights and also Christine Whitehouse from Uganda Cancer Trust visit us in Uganda. They brought such a sense of energy and encouragement and helped to give us a real impetus for our Cairdeas work. John Saxton, a pre-med student from the USA was also visiting us and is preparing a video we can share soon.
'My name is Felicity Knights and I am married to Dan (current Operations Director). Like Dan, I’m also a junior doctor, and together we’ve been friends of Cairdeas for more than five years and enjoyed sharing the journey. However, in July I had my first chance to actually meet the MPCU team and I loved it!
For me, one of the most exciting new developments is the new ‘Sanyu’ team that is supporting MPCU – Sanyu means joy. This team are newly trained volunteers from Kampala’s Lugogo Baptist Church, who are going to act as a community-based support team for palliative patients as they are discharged. MPCU’s volunteers are already an essential part of the team: giving practical, psychosocial, spiritual and practical support to patients and their families in Mulago, Kiruddu and Kawempe hospitals. The Sanyu team will help to extend care and pastoral and social support for patients holistically in their home setting.
Joy with the pigs....It was a highlight of the trip to visit the new pig farm project which has been initiated to try to provide a sustainable source of funds for the Sanyu team and the wider volunteer team. The project aims to breed and sell pigs, and all of the profits will go towards supporting the volunteer pprogramem as well as build capacity for incoem generation. I’m a trustee of another charity working in Uganda, Afrinspire http://www.afrinspire.org.uk/ who have offered some advice on this piggery, and in this role I have had the opportunity to visit a number of different agricultural and farming projects. So one of the things that really struck me about this particular farm was the dedication of the Farm’s caretaker (Senga), and MPCU volunteer, Toko, who has been overseeing the implementation of the project. Both were clearly determined to make the piggery a success, and believed strongly in the value of the project to support the Sanyu team in the work they are doing for MPCU. Senga shared with us that she saw caring for the pigs as God’s work, and that her faith was the thing that was driving all her actions.
Piggeries are actually one of the most rapidly-growing sectors of farming in Uganda at the moment, but setting one up is not without its trials! Unfortunately, the team have found themselves confronted with a number of challenges common to this sort of project: difficulties in finding land to farm, fluctuating prices of feed and breeding stock (in part due to Ugandan drought), and things just taking a lot longer to get started than originally hoped!
But it was wonderful to see where they have got to, and to discuss plans to take things to the next stage. One of the two piggery buildings was fully constructed, and we were able to see the four pigs inside: one boar and three sows, two of whom are currently pregnant, so it won’t be long till the first piglets come along! The next stages are likely to include completing the second building, purchasing some more sows, and starting growing food on the nearby land to help protect the project against the fluctuating food costs.
So it was a joy to learn about the Sanyu team and their piggery, and I’m very much looking forward to re-visiting and seeing the next stages come into fruition!'
Thanks Toko, Ivan, Grace and the whole volunteer and pig project team. We are doing this to enable us to care for more people in need and you already contribute so much.
Thanks also to UCT http://www.ugandacancer.org.uk/ who have been our main funder for this project. In particular Christine Whitehouse, has been such an amazing support for MPCU and for our Pig project in particular. Her business acumen has been invaluable with ongoing committment as well as the encouragment of visits from Micheal and Liz Minton who are trustees of UCT. Thanks...and looking forward to continue to being partners!!
You can get involved in supporting this project too by donating online through the Cairdeas website www.cairdeas.org.uk. Watch up for more updates and we will be offereing a chance to sponsor / buy your own pig soon. Some are already named...spot Catriona
Sanyu team

International colleagues joining Sanyu team

Growing, happy pigs ?Catriona

Site visit

Wonderful, faithful Senga

4 and counting

Toko, Ronald and Christine; thanks UCT for all your support
Mauritania; understanding rural communities and palliative care
![]() Cairdeas
Cairdeas
![]() 15th July 2017
15th July 2017
Thanks to Dr David Fearon who leads Cairdeas Sahara and has given us this update on an innovative and creative project in Mauritania which extends palliative care with an emphasis on community understanding, rural development and poverty alleviation.
'I am delighted to report the completion of a 12 month capacity building project in Mauritania. These activities were sponsored by Johnson & Johnson and managed by the Tropical Health and Education Trust (THET). The highlight for me was the multidisciplinary and international collaboration. Visitors represented France, Senegal, Switzerland, Uganda, UK and Sudan. It was especially nice to be able to host the country’s first palliative care training in Arabic during the visit by Dr Nahla Gafer and Dr Mohja Khair, Cairdeas friends from Sudan. I was relieved that their dialect of Arabic was easily understood, and it was wonderful how they identified so many similarities between these two countries of the Sahel, both in the environment and culture. I think they were jealous of our wonderful beaches!
Overall we training 75 health care workers from all over the country in the foundations of palliative care, and we visited nine of these participants for mentoring in their rural work setting. To gve an example one nurse said 'I was caring for an elderly man with cardiac failure. He had multiple pressure sores and dirty sheets. He was depressed. I dressed the pressure sores and showed the family how to do the same, in employing what he learnt during the training. I could see how I made a positive change in this man’s life and that of his family. The patient remained well until his death. I never say ‘there is nothing more that can be done’ anymore.”
At the moment, I am working with a French anthropologist on writing up the research which ran alongside the project. Unfortunately this means reading and rereading through the French transcripts of nine focus group meetings and 31 individual interviews. Eventually, we plan to publish two articles from this research. The first will be an anthropological reflection on the training and the effects of the training, and the second a discussion on the cultural ideas of death, dying and end of life care. I am already finding some good insights into how the concept of palliative care is viewed locally. For example, the definition of palliative care is centred around the idea of ‘life-limiting illness’ however this is a new concept for many Mauritanians, including health care workers. As one imam said : ‘it is not the illness which causes death, and it is not health which causes life’. In Mauritania, people believe that it is only God who is in control of life, health and death. A doctor or nurse who talks of an incurable disease may be considered as putting themselves in the position of God, or they may just not be aware of the available cure. Another aspect is that life is thought of as fragile and that most people have experienced suddenly losing a healthy member of their family, even while a severely ill family member makes a full recovery. Whilst we may think that these beliefs may lead to a fatalistic acceptance, in practice people feel a great burden to pursue any possible cure, whether through modern health care or traditional. At times this leads the family into debt as they continue their search for a cure.'
The THET website has also featured this project http://community.businessfightspoverty.org/profiles/blogs/john-paul-creating-responsive-not-prescriptive-global-health. This shows how we can partner to make a real difference...many thanks to all our Mauritanian and international partners and to Johnson & Johnson and THET for their grant..

Nouakchott beach

Presenting the certificates

Smiles and certificates

Active participation

Great team work as trainers

Sudan vs Mauritania football match..an unexpected addition to the trip
EAPC 2017 conference…..summer in Madrid
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 12th June 2017
12th June 2017
The EAPC World Congress 18th to 20th May in Madrid was a great event encompassing cutting edge education and research, networking, social interaction, meeting and renewing colleagues and friends, presenting our work and being inspired. It was so good that Dr Jack Turyahikayo was awarded an IAHPC Travelling Fellowship to attend and he shares more below...along with Dr Lucy Robinson who volunteered with us last year. We were presenting work which included a reveiw of our research capacity and I will write more of this in another blog.
All our posters and presentatons will be in our website folder under EAPC. We were very honoured to accept an award for Leadership led by Julia Downing and with Liz Grant which and recognised the amazing Leadership Fellowship for Nurses completed recently with the University of Edinburgh, Makerere University and PCAU. Great to also see one of our Cairdeas Trustees ; Hamilton Inbadas and see Dr Lungagowda from Kidwai in Banaglore accept a pprze. So good to share with our Malawi friends (Jane Bates) and Sudanese (led by Dr Nahla Gafer). We shared in the launch of the Atlas for Palliative Care in the Middle East and Africa; again these will be available in our Resources section very soon. It was so good to see the interest in refugee and migrant health and many many new ideas going forward.
Jack says: 'The EAPC congress 2017 will always remain such a memorable one for me. This was the biggest congress that I have attended with over 2000 participants from various countries. Presenting work on “Outcomes of care among patients referred for specialist palliative care in Mulago hospital” allowed me interact, share knowledge and practices with the greatest researchers in palliative care. I enjoyed the numerous poster and oral presentations which immensely positively impacted my research knowledge and skills. Many palliative care researchers were pleased with the work presented and stimulated ideas to better my PhD research that I intend to undertake. I was inspired to have more impressive work at the next EAPC congress in Berlin. It was such a pleasure that as a team, three of our posters presented emerged among the best in the various categories.
Touring Madrid City showed me the wonders of living in Madrid. The late dinning night life with thousands of people walking and touring was such an interesting experience for me. The Santiago Bernabeu stadium that I have always watched on TV has an amazing history in club football. It was joyous to visit this stadium seeing several trophies and accolades won by the greatest soccer players in club football. I also posed and lifted the most recent Champions league trophy won by Real Madrid. I particularly enjoyed Spanish food served as Tapas. The sea foods including squid, prawns, octopus and cray fish are all tasty dishes that left me mesmerized and wondering if I could find similar dishes back in Uganda.
Barcelona city was such a lovely and memorable experience for me too. The amazing architectural designs of the buildings were such a wonder to see. The Basilica Sagrada Familia by Gaudi marked by artistic sculptures of the Holy Family was the most beautiful cathedral I have seen. Park Guell overlying Barcelona city allows for an awesome view of most of the city. There was also a lot to learn about Gaudi`s work from this same place. The long walk along the La Rambla Street viewing many touristic places and spending time at the Barcelona beach was historical for me. I will always treasure these moments.
I also spent time at the University of Barcelona and learnt so much about its history. Visiting the Institute Catalagia Oncologia(ICO) that provides cancer care allowed me witness firsthand how patients with cancer are managed. I was able to see how chemotherapy is reconstituted and packaged by two robots supported by pharmacy technicians. I visited the palliative care team in this hospital which provides highly specialized services to patients and was pleased to see how it efficiently provides care to over 1000 patients a year. I easily appreciated the different contexts in which we all provide the much needed care to our patients.
I appreciate everyone who made it possible for me to have such a wonderful and unforgettable experience at the EAPC congress in Spain. Special mention goes to Dr Mhoira Leng who ensured that my stay in Spain was historical. I pray that God continues to provide the resources needed to thrust palliative care forward.'
Lucy adds her perspective: 'I am a doctor from the UK who volunteered with Cairdeas last summer at Makerere Palliative Care Unit (MPCU) in Kampala, Uganda. It was a challenging but enriching experience for myself and my partner John to give up our comfortable lives in Newcastle and travel to Africa. It really changed the way we look at life and work and we had some great experiences that we will remember for ever and met many inspiring people.
As part of this placement, myself and another volunteer, Dr Bex Cordner, undertook a project into research capacity building with the expert supervision and guidance of Dr Mhoira Leng, the Medical Director of Cairdeas, and her colleagues Dr Liz Namukwaya, Professor Scott Murray, Dr Liz Grant and Professor Julia Downing. Since MPCU was founded they have included research and evidence based practice as a core part of their academic Palliative Care Unit and have promoted a culture of research where everyone, from doctors to volunteers are encouraged to take part. This research provides evidence with which to deliver high quality Palliative Care in this setting and also helps the Unit to both achieve its strategic plan and measure its outcomes.
Our project, which I presented at EAPC in Madrid aimed to evaluate and measure the outcomes of this research culture and research capacity building through training. The study showed excellent results, with a large number of MPCU abstracts being presented at national and international conferences and positive outcomes from the research training delivered by MPCU.
The rest of the conference was incredibly interesting with a large amount of high quality studies into different aspects of Palliative Care being presented. It was a privilege to learn from these presentations and meet some of the people who are carrying out this important work. I found myself considering in more detail aspects of palliative care which I had not before, such as compassionate communities, managing frailty as part of palliative care and the health economics of this specialty.
Madrid itself was beautiful and Mhoira, Jack, Nasur (from Hospice Africa Uganda) and I spent a very enjoyable afternoon, after the conference, exploring. We marvelled at the stunning architecture, ordered way too many churros and accidentally joined a Spanish political demonstration!'
Many thanks to Cairdeas , IAHPC and THET for the financial support to allow us to attend and to all our wonderful colleagues who shared, inspired, laughed...but above all work for the development of palliative care, the relief of needless suffering and narrowing the health care inequity gap.

Warm welcome to EAPC 2017

Rosettes

Hamilton and our Indian colleagues with the prize winner Dr Lingagowda

African colleagues as the African Atlas is launched

Jack presenting his poster

Jack discovering seafood

Lucy presenting our work

Lucy and Jack and their proud mentor
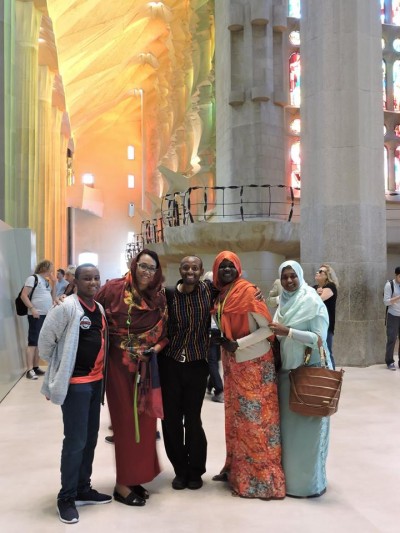
Beauty in Sagrada Familia with Jack, Nahla and our Sudanese friends
