
Meet the Scholars - Phillip Amol Kuol
![]() Cameron Don
Cameron Don
![]() 6th February 2025
6th February 2025
Meet Phillip Amol Kuol, one of our Cairdeas scholars! Phillip is currently in third year at Uganda Christian University in Arua, studying for his Bachelor's Degree in Social Work and Social Administration. We asked Phillip to share some of his story and his plans for the future.
I am a committed individual originally from South Sudan but currently residing in Northern Uganda. I have faced significant challenges, growing up as a refugee due to conflict in my home country. Despite these hardships, I have been relentless in the pursuit of education and am currently in the third year of study for my Bachelor’s Degree in Social Work and Social Administration and I have a great passion for serving my community.
I began my journey by working as a translator in Nyumanzi refugee settlement in Adjumani district, assisting South Sudanese refugee patients in Nyumanzi Health Center, and in the community. This position allowed me to develop a strong connection with the healthcare system. My interactions with healthcare professionals, particularly those focused on palliative care, inspired me to pursue further training, such as holistic care and counselling.
Phillip shared more about his work in Palliative Care.
My dedication and interest in palliative care led me to volunteer for the Village Health Team palliative care training, under the Transform Project with Medical Team International. Here, I received extensive training that equipped me with the knowledge and skills to make a significant impact in my community, particularly in providing care and support to adolescents, the elderly, my fellow refugees and the host community of Adjumani district.
Due to the knowledge I gained from palliative care training with Peace Hospice Adjumani, I became a volunteer for youth advocacy and a peer educator at Reach a Hand Uganda, where I worked in WAY project (Women, Adolescents, Youths Rights and Empowerment programme), U-decide, and Generation Gender project.
I also became the Executive Director of Dongriin Foundation, which is a refugee led organization in Dzaipi Sub County in Adjumani District. This has also added more capacity building, empowerment skills, experiences and knowledge to my growth.
Phillip went on to discuss his education and shared how the Cairdeas scholarship has helped him in pursuit of his goals.
My commitment to social work caught the attention of Cairdeas, an organization dedicated to promoting high-quality palliative care in resource-limited settings. Through their scholarship program, I was able to pursue a Bachelor's Degree in social work and social administration at Uganda Christian University (UCU). Unfortunately, the Adjumani Teaching Centre branch of UCU closed, leading me to continue with my studies at the UCU Arua Campus.
I am currently in the third year, second semester as a Bachelor's student at Uganda Christian University in Arua, Uganda. My coursework not only focuses on social work but also includes social administration and community health. I am deeply committed to my education, and to improving the lives of the voiceless in my community and promoting peaceful co-existence among youths, particularly within the refugee and host communities.
I wish to appreciate the team of Cairdeas for their great support rendered to me, I will give it back to my community and the world at large. I hope this support will continue to bring up more youths, to change my community and the world at large.
Finally, Phillip shared his plans for the future.
I wish to continue with my education up to Master’s so that I can add more knowledge through developing my career. I wish to work with authorities like Cairdeas and international organizations so that I will have more skills to become an international youth advocate. Besides, I would like to become an international worker so that I can also support refugees from other parts of the world as a way of giving back.
My journey is a remarkable testament to resilience, dedication, and the spirit of giving back to the community. My experiences and future aspirations demonstrate my unwavering commitment to making a difference in the lives of those around me.
If you would like to know more about Phillip's work, please email us at operations@cairdeas.org.uk



Hope Will Always Have the Final Word
![]() Cameron Don
Cameron Don
![]() 20th December 2024
20th December 2024
Our Medical Director, Dr Mhoira Leng, shares her end of year reflections for 2024.
As the year draws to a close let me take a moment to reflect.
At this time, many of us will be singing Christmas carols, and a much loved favourite is O Little Town of Bethlehem. The carol focuses on the events in the town of Bethlehem over 2000 years ago that would have historical and global significance. This part of the world was experiencing conflict, occupation, forced displacement, the killing of children and fear…then and now. Perhaps you will remember the powerful image from the Christian Church in Bethlehem of the nativity with the baby amidst the rubble wrapped in a kufiyeh and Rev Munther Isaac’s sermon; 'Christ under the rubble'.
As the carol says; ‘the hopes and fears of all the years are met in Thee tonight’
With devastating and ongoing conflicts affecting our partners in Gaza and the rest of Palestine as well as in Sudan our hearts are heavy. We have heard from Dr Khamis Elessi and other dear friends who continue to offer care to patients and families even as their own families are struggling to simply survive. We mourn the killing of dear friends and colleagues and the almost total devastation and destruction of the health system, the education system, systematic starvation alongside everything needed for life and for dignity. We are aghast as international and humanitarian laws are seemingly ignored and the whole foundation of our world order is under threat. When the voice of peace and hope seems unheard and ignored it can seem as though humanity itself is under threat.
Words from Munda Nasser, written in Advent reflections from Bethlehem, have been a support for me. She speaks of hope and reflects on these bible verses; ‘For in hope we were saved. Now hope that is seen is not hope, for who hopes for what one already sees? But if we hope for what we do not see, we wait for it with patience.’ ROMANS 8:24-25. She says; ‘The Christmas story is a reminder for humanity all over the world to reorient its compass and ask: What can we do to build hope, to reconstruct it collectively? Sumud forms our collective Palestinian response to the everyday systematic oppressions that we go through. It forms our stand and our journey toward what we cannot see. It forms our inability to sit with hopelessness —it is a way of saying that hope will always have the final word.’
So what gives me hope as I look back on 2024. I see the amazing way Cairdeas partners are working in challenging situations where resources are constrained and needs can be overwhelming. I see the innovation, resilience and compassion to deliver training, research and clinical care in Uganda, Sudan, Gaza, Mauritania and India. We read the essays from medical students reflecting on holistic care learning in the midst of conflict in Gaza. We hear of the impact our Scholarships have had for inspirational colleagues such as Toko, Vicky, Liz, Philip and Ronald in Uganda. Our Compassionate Leadership Fellows in India are being transformed and already putting their learning into practice. (Please go back and listen to the videos from our Cairdeas Gathering to be inspired) I am humbled by the many who give their time and expertise in the Cairdeas Faculty and those who give, volunteer, pray and support in so many other ways.
At the heart of Cairdeas is the dignity of the people who face each day living with serious illness and who walk in the twilight days of their lives. Palliative care seeks to accompany people on that journey and focus on listening to concerns, alleviating suffering, supporting quality of life, promoting dignity and being in solidarity for justice. This is the heart of compassionate palliative care. This is the heart of humanity.
Let me mention one project we are focussing on this year for funding support. ‘Sunshine During War’ was formed by Dr Nahla Gafer and colleagues from Sudan in partnership with Sanad Home Hospice Care in Lebanon and CairdeasIPCT. It has brought psychological support for staff, patients and families, offered clinical mentorship and expert support and helped to sustain services within war torn Sudan through practical help for internet access, travel and even at times food and basic living needs. We are now extending this to include Gaza - led by Mervat Hammad, one of our Diploma students, now in Egypt. We will be sharing more of this project soon. Let us hear from Nahla…
‘Yes, we helped them, they needed us, but also, we needed to preserve the work that we had started; we needed to help our patients. It is part of who we are. This way we are really healing, caring and humane health professionals.’
Please consider gifting towards this programme now or in the future. You can do so here.
So wherever you are and however you are feeling at this time of year may we all be inspired, renewed, energised and encouraged to live with hope in hearts full of gratitude.

Christ Under the Rubble

Church of the Nativity

Stars in the Street
Gaza, 76 years on
![]() Cameron Don
Cameron Don
![]() 22nd October 2024
22nd October 2024
Author: Dr Mhoira Leng
At this time we are remembering the terrible suffering of the people of the land and the ongoing suffering of the Palestinian and Israeli hostages as well as the hundreds of thousands of displaced, the bereaved, the injured, those who struggle to find hope in the midst of such hopelessness.
This poem from Khawla Badwan speaks so searingly of the many, many years of pain and suffering. Read it with your heart.
Words can be difficult to find. I have found solidarity in sharing the words of our colleagues and friends in Gaza; people we have worked with for over a decade and even now show such courage and compassion even as they cry out to a deaf world to end the suffering.
‘Where we were displaced was in Mawasi Khan Yunis. From morning to afternoon, we died a thousand times from the very high temperature and the hot weather. We have reached the point of pouring water on our heads as we sit to endure the heat. Even the water is hot from the high temperature, and we also drink it warm. What misery we are living in, what fate still awaits us. We are crushed, sadness consumes us. To God only we raise our palms. From the misery of the Gaza Strip, we are still calling out: We have the right to live.’ Randa Said, nurse.
We are part of a humanitarian movement that seeks to advocate for the needs of our brothers and sisters and for the world to ensure humanitarian law is respected even or especially in times of war. This means the protection of all civilians, access to healthcare, protection for healthcare workers and access to food and water at the very least. I have been privileged to speak and share the words and experiences of our Gaza colleagues in many forums; from international cancer conferences, to palliative care events and solidarity events. We continue to explore how to better support those with non-communicable disease and palliative care needs in conflict zones through these forums and with PallCHASE.
A few weeks ago we came together as International and Gaza faculty to repurpose the pain and palliative care course materials for the Islamic University of Gaza. By making these low-bandwidth, asynchronous sessions with embedded case scenarios we were able to support students, who were studying in the most challenging of circumstances, continue their education. We are grateful to the Gaza Educate Medics platform and PalMed, who are supporting a board international network to continue the medical school curriculums online. The Deans of both medical schools are leading the Gaza faculty and guiding the international community. Our students had never had their clinical training induction so worked hard to complete the sessions, the exams and the case reports. They sent me a few photos of their studying conditions. What courage to continue to prepare to be the doctors so needed by their own people!
When I left Rafah in April 2023 it was with a deep sense of foreboding that the world would not stand with the red lines; that Rafah and all the hospitals, clinics, displaced population and wonderful people would be overrun. And so it happened…courageous compassionate people left to struggle in tents which now flood as the weather turns again. Who search for freedom for dignity, for the basics of life and who still find the courage to rebuild hospitals and clinics, to care for those in need, to study and complete exams…to hope.
Palestinians speak of a core value, samud or steadfastness and this is humbling to see yet they also tell us of their exhaustion.
‘We are not well. We can no longer continue, to continue as if nothing has happened. Our hearts hurt because of the weight of what they carried inside them, and our bodies are exhausted because we did not find a safe space in which to retreat. We are tired of concealment, because we are not accustomed to revealing what makes us sad. Our tears used to fall, exposing what we hid. A lot. We feel very tired, but we pretend to resist. If these days pass quickly, we will sleep for a long time. We have no energy to endure anymore. We are tired and every part of us is tired.’ Suha Suleiman Shaath, pharmacist.
When I speak to my dear Palestinian brother, Dr Khamis Elessi, the first thing he says is ‘we are still alive’…he sends his greetings and longs for the war to be over and for people to know the true nature of what they are experiencing. He concluded his message with the words. ’May the sun of hope, freedom, justice and peace shine again.’
May God protect and sustain him, his family and all our brothers and sisters in Gaza and also in Palestine, Lebanon and Israel to bring a just peace to all the land. Let us come together as one humanity to find and demonstrate a different way.
Let me end with a prayer from the Archbishop of Jerusalem, Hosam Naoum, writing last week on the anniversary of the bombing of the Ahli Christian Hospital in Gaza City.
A Prayer for Peace and Healing
Great Healer, we lament the horrific wounds and loss deep beyond comprehension. Repair and restore hearts wounded by unimaginable fear and trauma. Provide a way for healing for the multitude who are injured in body and spirit. May your people and the earth know your mercy and an end to the suffering. May your healing compassion be manifest among creation and the people of the earth. Amen.
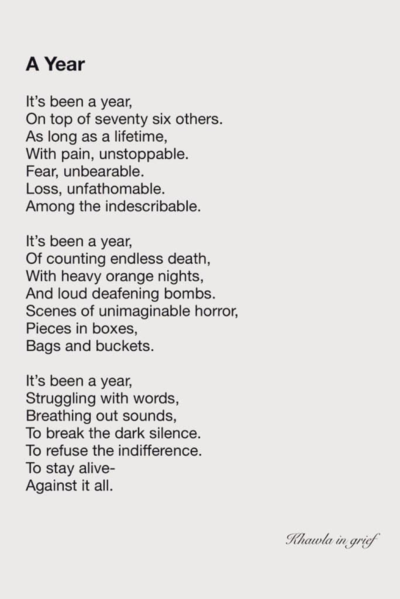
A Year by Khawla Badwan

Clinical examination taking place in a corridor

Studying continues in Gaza

Working and studying conditions continue to deteriorate

Suha Suleiman Shaath, pharmacist
