
Meet the Scholars: Vicky Jemimah
![]() Cameron Don
Cameron Don
![]() 17th October 2025
17th October 2025
Cairdeas is pleased to be welcoming two new scholars into our scholarship program this year. The scholarship program has been a key part of our mission to improve the skills of ‘in-country’ health workers, allowing our partners to lead the way in improving access to palliative care in their home countries.
One of these new scholars is Vicky Jemimah, a long-standing volunteer with PcERC, our partner organisation in Uganda. Vicky will be undertaking a Degree in Social Work at Victoria University, Kampala.
Vicky wrote to the Cairdeas, expressing her appreciation for the scholarship, telling us about her plans to improve the lives of her patients through this degree, and introducing herself to our supporters.
I want to take a moment to express my heartfelt gratitude for the scholarship you've provided me to pursue my degree in Social Work and Social Administration. Your generosity has made a significant impact on my life, and I'm deeply thankful for your investment in my future.
I'm Vicky Jemimah, a dedicated social worker currently working as a volunteer social worker with the Palliative Care Education and Research Consortium unit in Mulago hospital since 2018. I got to join this wonderful team through my mum, who was a link nurse working under Mulago hospital, and I can gladly say it’s one of the most beautiful journeys I have experienced.
I am passionate about empowering vulnerable populations and advocating for those in need. I care for patients and their carers/families by providing physical and spiritual support and counselling them during difficult times. My aim with this degree is to enhance my skills and knowledge in social work, ultimately improving the lives of patients and families I serve. I'm committed to applying the knowledge and skills gained from this program to provide more effective support and services to my patients, particularly in areas such as patient advocacy, counselling, and community resource coordination.
Vicky’s words are backed by her recommendation from Elizabeth Nabirye, the clinical lead of PcERC, who described Vicky as holding “an unwavering commitment to social justice and community development” and praised her work in research, advocacy and counselling, which “reflects a genuine dedication to improving lives and strengthening communities.”
Vicky continues, speaking on the impact of the scholarship to her,
This scholarship comes at a pivotal moment in my life, bringing hope and renewed purpose after a challenging period of separation from my husband and marriage with our 2 lovely boys. The support of Cairdeas has not only alleviated financial burdens but also restored my faith in my abilities and future prospects. I'm grateful for the opportunity to focus on my studies, develop expertise in healthcare social work, and advance my career.
To the members and supporters of Cairdeas, thank you for believing in me and supporting my education. Your kindness and generosity will empower me to create a brighter future for myself and those I care about. Your contribution will have a direct impact on the lives of those I serve, and I'm grateful for your trust in me.
We would like to reiterate Vicky’s thanks to the Cairdeas supporters. Your donations allow us to run projects like the scholarship programme, making a difference to lives on the ground and further advancing the development of palliative care leadership in our partner countries. We wish Vicky the very best as she begins her studies and can’t wait to see her development as she progresses through the course.

Vicky Jemimah, our new Cairdeas scholar

Vicky at work as a volunteer social worker

Vicky is a long standing volunteer with PcERC, our partner organisation in Uganda

We are delighted to be supporting Vicky as she pursues her degree!
Sojourn in Helsinki; European Association for Palliative Care Congress
![]() Cameron Don
Cameron Don
![]() 11th September 2025
11th September 2025
Representatives from Cairdeas travelled to Helsinki earlier this year to attend the 19th World Congress of the European Association for Palliative Care. Dr Mhoira Leng, Dr Chitra Venkateswaran and Dr KV Ganpathy represented the UK and India branches of Cairdeas, presenting posters and giving presentations across various areas of work.
This is a major event in the global palliative care calendar with 1759 participants from 75 countries coming together. There were 776 abstracts, 280 speakers and 625 e-posters. The city hosted us with a glimpse into the rich culture and heritage of Finland.
The areas of research and findings presented by the team were:
It’s a huge honour to present these areas of work from India and Uganda and to listen and interact with others; building understanding and collaboration. We recognise the hard work and dedication and thank all those who have contributed to carry out and compile research findings
Dr Chitra reported that the conference was of great benefit to her and her work:
“I was able to learn from a number of posters, which brought learning and ideas on research on diverse topics in palliative care. I was also able to meet many experts and seniors in palliative care. There were many innovative themes and formats in the conference which we could adapt to our settings…such support to professionals from low-middle [income] countries provide great opportunities to witness and carry home important insights to adapt and deliver from such global events.”
Dr Mhoira had the immense privilege to present a plenary on behalf of Dr Nahla Gafer, who was not able to travel due to her own displaced status from Sudan; especially disappointing given the topic. ‘Caring for refugees and migrants: what is the role of palliative care?’ See the plenary presentation here
‘We set the scene showing that 117 million people are forcibly displaced; more than at any time in history. Many are displaced by conflict, though climate change is a major factor in forced migration. One of the most significant and concerning aspects of conflict settings is the increasing direct attacks on health and healthcare. 14 countries report such events this year alone (https://extranet.who.int/ssa) and countries such as Ukraine, Myanmar, Sudan and of course Gaza report the devastation this causes. A recent report ‘In the Line of Fire’ contains important global information and a call to action.
We told of one palliative care nurse in Sudan who was taken from her home at gunpoint to treat injured militia and at great danger to her life. We told of the 3.5% of Gaza’s health workforce who have been killed or taken into detention with almost complete destruction of the health facilities. This includes access to pain control, so essential for palliative care.
We share poignant stories from our palliative care colleagues in Sudan, where colleagues are using virtual means to offer staff-patient support through the Sunshine During War project led by Dr Nahla Gafer. Find out more about Sunshine During War here.
We called for a commitment to humanity, and for the global healthcare community to stand in solidarity with their colleagues, who every day are trying to care for their patients amidst violence, destruction, starvation and direct attacks. We appealed for international law to be upheld without discrimination. The rousing applause was heartening and powerful with many conversations afterwards showing the depth of concern and compassion.
Dr Ganpathy also shared his reflections on the conference, in particular how it helped him to see where colleagues in similar contexts worked creatively to care for their patients;
‘Attending EAPC (European Association for Palliative Care) conference is crucial for professionals in the field as they offer opportunities for networking, knowledge sharing, and professional development.
EAPC 2025 held at Helsinki from May 29-31 in particular was designed with enriching sessions both medical and psychosocial. The congress served as a global forum for interdisciplinary education, research, and professional exchange. Coming from a Low and middle income country(LMIC) I could understand how some of the facilities from other LMIC’s are creatively meeting the demands of patient care. The conference showcased the latest research findings, practice-changing science, and emerging trends in palliative care.
The events saw a convergence of physicians, nurses, researchers, allied health professionals, and volunteers, Creating a unique platform for attendees to connect with &, build relationships, and foster collaborations.
The Q&A session after every presentation was one of the engaging aspect of the conference. A dedicated session and a plenary on children's palliative care, had me reflecting on our own practices back home.
In essence, attending EAPC conferences is an investment in professional growth, knowledge advancement, and the overall development of palliative care.”
We are thankful for the opportunities to travel and represent Cairdeas at these important global forums. Thank you to all of our supporters who help to fund this work, and deliver the message of compassion and humanity to colleagues around the world.

Drs Mhoira, Chitra and KVG with their presentation posters at EAPC 2025

Drs Mhoira and Chitra meeting with colleagues and friends

Dr Nahla Gafer delivers a short introductory message to the plenary
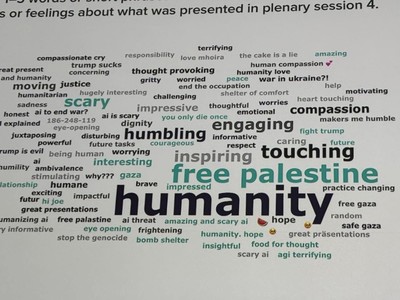
An audience wordcloud generated following Dr Mhoira's plenary
Compassionate Leadership Fellowship: The Fellows’ Retrospective
![]() Cameron Don
Cameron Don
![]() 2nd July 2025
2nd July 2025
In February this year, the Compassionate Leadership Fellowship came to its conclusion, marking the end of a year of growth, learning and development for our cohort of palliative care leaders from across India, Nepal, Kenya and Rwanda. I reached out to two of our fellows, George Varghese and Keshav Sharma to ask them about their experience of the CLF course and to find out what impact it has had on them, personally and professionally.
Firstly, George and Keshav introduce themselves and their work to our readers and supporters.
George
Hello, I'm George Varghese, a highly experienced healthcare leader with more than two decades of experience, cutting across palliative care, hospital administration, and community-based public health. I am presently working as the Director of Community Health Projects at Kachhwa Christian Hospital, Uttar Pradesh, overseeing multi-village interventions for communicable & non-communicable disease and palliative care.
Keshav
I’m Keshav Sharma, Psycho-oncologist and Grief therapist with over a decade of experience supporting patients, caregivers, and healthcare professionals across India. My work lies at the intersection of mental health, palliative care, and compassionate leadership, and I’m deeply committed to creating spaces of dignity, presence, and healing in cancer care.
I’m focused on integrating mental health into palliative care through presence, dignity, and culturally sensitive care.
Beyond clinical practice, I find deep meaning in teaching what I learn from the therapy room. I’ve had the privilege of mentoring hundreds of students and professionals and serve as faculty for national and international palliative care training programs. For me, sharing knowledge is a way of sustaining the work of planting seeds of empathy, dignity, and presence in those who care for others.
- What impact has the CLF had for you?
George
The Compassionate Leadership Fellowship (CLF) has profoundly and multifacetedly impacted both my personal and professional life. It provided a structured process for deep self-evaluation, helping me become more self-aware and intentional on my leadership journey. The course fostered a safe space for reflection and growth, leading to significant positive changes in my relationships—especially with my daughter—and in my emotional resilience. It helped me recognize unhelpful patterns like perfectionism and taught me to embrace vulnerability, humility, and authenticity. Most importantly, it instilled in me a renewed sense of purpose and a stronger, values-driven leadership identity. The CLF has been a transformative journey for me. It was not just a training program but a deeply personal and spiritual experience. It acted as an eye-opener, leading to profound self-realization and a deeper understanding of others. Each session challenged and equipped me to face greater challenges in life with empathy and strength. The stories shared, the bonds formed, and the lessons learned have left a lasting impact on my heart and mind. CLF didn’t just educate—it healed, inspired, and provided me with a new lens to view myself and the world around me.
Keshav
Compassionate Leadership Fellowship has had a profound impact on my approach to both my personal and professional journey. The fellowship helped me integrate compassion into the structural framework of my leadership style, rather than viewing it merely as an emotional response.
The most profound impact has been the recognition that vulnerability and strength are complementary rather than contradictory. Working in psycho-oncology along with grief therapy, I've always acknowledged the emotional weight our patients carry, but I previously maintained professional distance as a leader. The fellowship taught me that authentic leadership requires embracing my own humanity and sharing appropriate vulnerabilities with my team.
This paradigm shift has allowed me to create deeper connections, both with patients facing cancer diagnoses and team members navigating the emotional complexities of clinical work with the patients. I have moved from a mindset of "leading from the front" to "walking alongside" my team, which has fostered greater trust and collaboration.
Another important area of learning for me was on role of mentorship, owing to how my mentor guided and mentored me through the process of learning throughout the year with his patience and presence.
2. How has the CLF changed you as a leader?
George
CLF has completely transformed my approach to leadership in both mindset and practice. I have become more reflective and patient, choosing to listen deeply and act with compassion rather than react impulsively. The Leadership Practices Inventory (LPI) and tools like personality and conflict style assessments have helped me identify key areas for growth and develop a leadership style grounded in empathy, courage, and collaboration. I now prioritize nurturing others, aligning with team strengths, and creating space for shared decision-making. The mentorship I received has also built my confidence and provided me with a clearer, more strategic approach to navigating challenges. CLF has allowed me to rediscover and redefine myself as a leader. It has illuminated previously concealed aspects of my leadership journey and clarified my purpose. I have learned that vulnerability is not a weakness, but a powerful strength. I now approach leadership with greater empathy, humility, and authenticity. Observing the diverse teaching styles of various mentors and learning from their heart-led leadership has inspired me to lead with compassion, integrity, and boldness. I have embraced my brokenness and use it as tool to encourage and uplift others.
Keshav
The fellowship has reshaped my leadership identity in several meaningful ways:
First, I have developed a more nuanced understanding of strategic planning that balances organizational objectives with human considerations. Before the fellowship, I often approached challenges primarily through the lens of efficiency and clinical outcomes. Now, I incorporate the emotional and interpersonal dimensions into every decision-making process.
Second, the mentorship component was transformative. Observing established leaders in palliative care demonstrate vulnerability while maintaining effectiveness challenged my preconceptions about authority. I learned that acknowledging limitations and seeking input creates stronger solutions than projecting infallibility.
Third, I've become more intentional about creating psychological safety within my team. The conflict management component of the training provided practical approaches for addressing tensions in ways that honour all perspectives while moving toward resolution. This has been particularly valuable in the emotionally charged environment of mental health professional work in palliative care.
Finally, I've embraced a more balanced view of leadership that values grassroots involvement alongside strategic direction. The fellowship helped me recognize that effective leadership in palliative care requires both vision-setting and direct engagement with day-to-day realities.
3. How have you seen the skills learned on CLF impact on your work?
George
The skills and insights I gained through the CLF have significantly impacted my work. I have improved team dynamics through personality assessments and 360-degree feedback, and I have incorporated technology such as AI tools for more efficient project management. As a result, my leadership has evolved in every aspect. I am now better equipped to support the nursing team by identifying training gaps and providing hands-on orientation in palliative care. Our multidisciplinary team meetings, guided by SPICT indicators, lead to more thoughtful and coordinated care planning. Overall, I have witnessed the emergence of a more empowered, collaborative, and motivated team, driven by trust, clarity, and a shared purpose. The skills I learned in the CLF are already influencing how I interact with others and respond to situations in my work environment. I have become more empathetic and intentional in my communication and actions. I actively listen more, remain present with those I serve, and create space for meaningful relationships to develop. The leadership tools, frameworks, and personal stories shared during the training have enriched my ability to support, mentor, and accompany others on their journeys. My work now feels deeper, infused with a sense of purpose and compassion that I carry with me every day.
Keshav
The skills I gained through the fellowship have had a tangible impact on my daily work, whether in navigating difficult family conversations in a clinical setting, supporting colleagues through emotional burnout, or strategic planning for psycho-oncological services, I now approach each task with greater clarity, collaboration and compassion. Conflict management which once felt daunting is now a space for growth and dialogue. Strategic planning is no more just about outcome but about aligning efforts with shared vision.
With my clinical team, conflict resolution skills have transformed potential disagreements into productive dialogues. Recently, when team members had differing approaches to supporting a particularly complex grief case, I facilitated a conversation that honoured diverse perspectives while developing an integrated care plan that drew from multiple therapeutic approaches.
Organisationally, the strategic planning training has helped me develop more sustainable programs. A bereavement support initiative, which I developed during my fellowship as part of my Leadership Development Plan, intentionally addresses both immediate emotional needs and long-term healing through a carefully structured progression, resulting in better outcomes and resources which remain sustainable.
Perhaps most significantly, the emphasis on authentic leadership has allowed me to model compassionate presence for newer psycho-oncologists. By demonstrating that we can acknowledge our emotional responses while maintaining professional boundaries, I've helped create a culture where clinical excellence and human connection are equally valued.
The fellowship's focus on values-based leadership has been the most impactful part for me personally which clarified my decision-making process, particularly when facing difficult resource allocation questions. Having a clear framework for prioritizing compassionate care while acknowledging practical limitations has led to more consistent and principled choices.
Thank you to George and Keshav for sharing their perspectives on the CLF, and for making clear the value and effectiveness the course has had for its participants!

George Varghese

Keshav Sharma

George with mentor Dinesh and fellow Rontu, during the day trip to Mango Meadows

Keshav with Dr Mhoira and Dr Frank Ferris, part of the CLF leadership team
