
Palliative care Specialist Fellowship Programme in Uganda
![]() Hannah Ikong
Hannah Ikong
![]() 15th April 2024
15th April 2024
We are pleased to give some updates on the Palliative care Specialist Fellowship Programme, or the PcSFP, based in Kampala, Uganda. The PcSFP has been made possible through our partner the Palliative care Education and Research Consortium, or PcERC, which works in two national referral hospitals in Kampala.
Since March 2022, PcSFP plans were officially commenced with an international steering group and dedicated staff. PcERC, with a grant from Cairdeas IPCT, held an education coordinator position to develop materials and support the PcSFP steering group in the curriculum, framework, and programme proposal. Much has been accomplished and we now prepare for the accreditation and establishment of the PcSFP as the first specialist fellowship in palliative care in sub-Saharan Africa. Here’s what you need to know about the PcSFP (to date) and our next steps in launching the fellowship.
Curriculum and Framework
In our last update from July 2022, the initial workings of a curriculum were formed in a benchmarking and writing process by Drs Liz Namukwaya and Kate Howorth, overseen by Dr Mhoira Leng, the Cairdeas IPCT Medical Director. The Association of Palliative Medicine (APM) in the UK supported us to solicit experts of palliative care education in Africa to help design the knowledge, skills, and attitudes and behaviours listed in the curriculum. We also shared the curriculum for independent expert review in the UK as well as a senior faculty review from the Department of Medicine, College of Health Sciences at Makerere University in Kampala, Uganda. The final result is a twenty-page curricula document, rich of global expertise and Africa-specific applications, organised into four domains and twenty-five themes, with learning objectives and their relevant knowledge, skills, attitudes, and behaviours.
As the curriculum underwent final reviews, Dr Liz Namukwaya and Hannah Ikong prepared a competency framework aligned to the curriculum. This framework not only listed the standard for a fellow to complete each theme in the PcSFP, but the standard that must be met by fellowship instructors or lecturers themselves. Competencies are quite important measures in this clinically heavy PcSFP and all competencies include the important attitudes and behaviours associated with transformational learning.
Proposal for Accreditation
Our programme proposal has been built a layer at a time, drawing from deliberations from the international steering group of palliative care specialists in Uganda, the UK and Ireland as well as continued research into accreditation in Uganda. Colleagues who have founded similar sub-specialist clinical fellowships in Uganda (such as Cardiology, Onco-Gynaecology, and Pulmonology/Respiratory) have been helpful resources in sharing their approach to clinical fellowships and accreditation pathways.
Our proposal, originally written by Dr Kate Howorth in 2022, remains a living document as we discuss options with the Uganda Medical and Dental Practitioners Council (UMDPC) in country as well as the option of later expansion with the East, Central and South Africa College of Physicians (ECSACOP). Last year included networking and stakeholder involvement, such as when Dr Peace Bagahsa, board co-chair of PcERC gave a ECSACOP conference presentation for our fellowship in August, or Dr Liz Namukwaya and Hannah Ikong introduced the PcSFP to the Uganda Ministry of Health Assistant Commissioner in November.
Way Forward
2024 has quite a bit in store for the PcSFP! On the accreditation side, we plan to finalise discussions with stakeholders and host institutions in this year, so we can apply for accreditation with the UMDPC and, with time, ECSACOP. Conversations with other palliative care associations and possible education partners are paramount, as well as establishing the partnership with the Uganda Ministry of Health. We also continue to invite international collaboration and discuss virtual contributions such as recorded instruction or one-on-one mentorship of fellows.
In March 2024, the education coordinator for the PcSFP was handed over from Hannah Ikong to Bernadette Basemera, an experienced palliative nurse who has recently supported another institution to accredit their palliative care education programmes. The steering group committee, PcERC and Cairdeas IPCT are all excited to welcome Bernadette to the programme and support this crucial stage in the PcSFP.
As friends and donors of Cairdeas IPCT, we thank you for your continued support in our vision of a world where palliative care is accessible by all. The PcSFP will met the need for specialist palliative care physicians in Uganda and, we hope someday soon, in East, Central and South Africa regions through ECSACOP.
Acknowledgements
All figures included in this blog post are from the poster of "International collaboration between Uganda and the UK to design Sub Saharan Africa’s first Palliative Care Fellowship programme: mutual benefits and learning." The poster was designed in October 2022 for the Palliaitive Care Congress of the Association of Palliative Medicine by Dr Kate Howorth, Dr Elizabeth Namukwaya, Dr Kathleen McGeough, Dr Kalyani Snell, Hannah Ikong, and Dr Mhoira Leng.
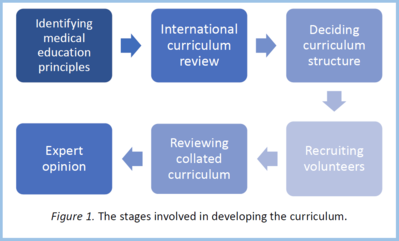
Figure 1. The stages involved in developing the curriculum.

Introducing Bernadette Basemera, the new education coordinator for the PcSFP.
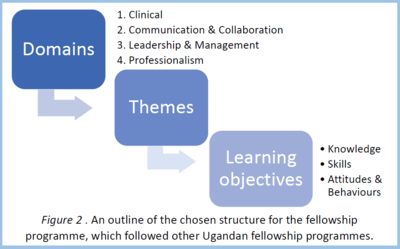
Figure 2. An outline of the chosen structure for the fellowship scheme, which followed other Ugandan fellowship programmes.

Dr Liz Namukwaya, one of the co-chairs of the PcSFP steering group committee and the consultant link in PcERC and Makerere University.
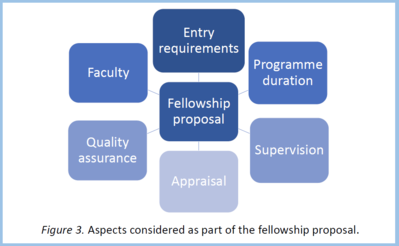
Figure 3. Aspects considered as part of the fellowship programme.
Six months till this moment: Report from Gaza City, Dr Khamis Elessi
![]() Cairdeas
Cairdeas
![]() 15th April 2024
15th April 2024
This blog post was shared as an audio message by the Cairdeas lead in Gaza, Dr Khamis Elessi. This is his message that he would like to share with all peace-loving people worldwide.
Hello, my dear friends, all of you, ladies and gentlemen. This is Dr Khamis Elessi, speaking to you from Gaza City. I have been living here in Gaza City since I was born here, but never in my whole life that I have seen something like this.
Not even my parents, not even my friends, not even senior people have ever seen something that we are experiencing at the moment. Since six months, to the moment, Gaza strip has been subjected to the most brutal, barbaric, relentless attacks from air, land, and sea from the Israeli forces.
Six months till this moment, 2.4 million Palestinians, who are being stranded for the last seventeen years in Gaza Strip under strict Israeli siege, have been subjected to the most brutal killing machines ever been witnessed in the last 200 years, more than what has been seen in World War II. Since six months till this moment, 2.4 million Palestinians have been forced to evacuate their homes at least six to eight times, evacuate their shelters, or the remaining parts of their shelters. Since six months till this moment, 2.4 million Palestinians have been subjected to the most moral and the most mental pressure ever experienced worldwide because of the intensity of the bombardment, because the amount of bombs dropped on every metre of Gaza Strip.
Gaza Strip has witnessed relentless attacks, 24/7, 24 hours, seven days a week, leaving more than 33,000 Palestinians killed, leaving more than 75,000 Palestinians injured. The vast majority of them are women and children, seventy-five percent women and children, and the remaining of them are elderly people or people engaged in fighting. The rest, the vast majority of Palestinians who were killed or injured do not have anything to do with fighting or with militance. Unfortunately, since six months till this moment, more than 80,000 Palestinian homes have been demolished completely and more than 300,000 have been damaged partially or mildly.
Over the last six months, more than 30 hospitals, out of the 36 hospitals all over Gaza Strip, has been made non-functional, uncapable of providing any sort of medical care for patients, and more than two million Palestinians are unable to access any healthcare of any type in their local residence. Since six months until this moment, more than 400 healthcare professionals have been killed, including doctors, nurses, physiotherapists, and aid workers.
Since six months till this moment, more than 160 journalist have been shot dead, more than 140 UNRWA staff, United Nations staff, has been killed as well. In addition to the bombardment, to the military onslaught on Gaza, there was a new weapon used on people who remained in Gaza City, which is starvation, starvation war.
So since three months till this moment, Gaza and the northern part of Gaza have been subjected to the most brutal starvation techniques, leading to famine among children and elderly, especially the fragile population and the marginalised population. So people were forced to eat cow’s feed, which is the only thing available on the market and if, if they still have the money to but it.
Unfortunately, prices have risen by twenty times, thirty times, forty times sometimes. So leading, just to give you one example, flour before the war cost one-third of a dollar, and now one kilo of flour costs $35, so that means 1,000% times increase in the price of flour, almost 500% increase in the price of rice, almost 300% increase in the price of other things. And name it, everything has increased between twenty times and 100 times the original price, and people here are running very low on money, so they could barely afford to buy food or buy anything, especially those who are not employed by Ramallah government, or Gaza government, or UNRWA, or United Nations, or international staff.
So those are left behind with no money and no food, starving, and we have witnessed so far the documented death of 28 Palestinian children who died of starvation and dehydration. What we need now? We need to stop this onslaught and we need to go back to peace and order, because peace is the only way that Palestinians and Israelis and Americans and British can survive on this earth, like brothers and sisters. And we need to bring medicines to those in need, especially patients with cancer, patients with chronic illnesses.
Imagine I’ve been helping at Al Shifa [since this recording this whole medical complex has been completely destroyed] and we’ve treated lots of children. Massive burns, that I have never seen before and without even morphine, and we know that those kids are going to die today or tomorrow because of the intensity and massive spread of burns all over their bodies and the depth of that burn. But unfortunately, even though we know they are going to die, they die in severe agony; so we do not have morphine, we do not have any strong analgesics to provide to them to alleviate their pain and suffering. And if they are going to die, there is no place for them to die because their families were kicked out of their homes many times, and their homes were burned so that they make sure that when they come back to their homes, they will find no home to stay in.
This is the strategy that they kick them from their homes, they burn their homes, so that they will be forced not to come back anymore to their homes or remain in places. Roads have been uprooted from their places so no ambulance can reach for the injured patients. Hospitals have been damaged, drugs have been banned, food has been banned. Electricity has been cut, communication has been cut, telephone communication has been cut. So, it is an intentional way of killing as many Palestinians as they can in the shortest time period while the world is watching.
Gratefully, the world is starting to wake up and see these massacres and they are calling for ceasefire, immediate ceasefire. But unfortunately the Israeli side is not stopping the killing machines all over Gaza Strip. And we hope that you and many free people worldwide, many peace-loving people worldwide, will act immediately to stop this onslaught on Gaza Strip and to open borders, and to allow Palestinians, women, children, girls, to live as equal as other international people in their countries. In peace, in order with neighbours, and in peace and in order with everyone worldwide.

Dr Mhoira Leng and Dr Khamis Elessi in Gaza in March 2023.

A picture taken in Northern Gaza by Dr Mhoira Leng before the war.

Happier times, when the Rantisi Hospital was operational in Gaza; the peadiatric unit with Dr Khamis Elessi.

Dr Khamis Elessi with Dr Amjad Eleiwa during one of the Professional Diploma in Palliative Care activities.

Dr Mhoira Leng with some of Dr Khamis Elessi's family last year. They are all in Gaza at this moment.
Reflection on Advocacy with WHO for Non Communicable Disease in Emergencies
![]() Dr Mhoira Leng
Dr Mhoira Leng
![]() 11th April 2024
11th April 2024
Non communicable diseases (NCDs) and emergencies are an area that can take a back seat when humanitarian emergencies occur. During such emergencies, the focus is on rescue and management of injuries. Yet we also know that the toll from illness such as heart attacks, strokes, lung problems, cancer, diabetes, and kidney disease will dramatically rise in an emergency where stress is everywhere and access to health care and essential medicines becomes impossible. Attending the World Health Organisation (WHO) Executive Board meeting as a representative of the IAHPC gave me an opportunity to explore these issues. As part of the 154th Executive Board of WHO, I read a Constituency Statement on behalf of IAHPC as well as gave an Individual Statement under the Global Health and Peace Initiative.
Across all this is the need for pain control, such as for those with advancing cancer, for those with burns and crush injuries, for women delivering babies, for those at the end of their lives and who need to die with dignity. Underpinning this is holistic care for patients, families, and staff: this is core palliative care.
Just stop for a minute and imagine being unwell in Gaza right now. There are almost NO strong painkillers like oral morphine available for ANYONE. So many factors lead to the lack of strong painkillers, but it is truly terrible and adds immeasurably to the suffering.
It was a privilege to attend the first WHO High Level Meeting on Non-Communicable Diseases in Humanitarian Emergencies in Copenhagen. So much work has gone into this, not least from the Eastern Mediterranean Office (EMRO) of WHO. It was heartening to see the member states attend (including Uganda) and many side events highlighting specific issues.
A recent report was shared which projected the risk of death and disease from NCDs in Gaza, but also infectious disease as the informal living arrangements are truly terrible. For example, right now in Gaza there is one toilet for 600 people and no clean water.
I took part in the Palliative Care side event and we had speakers either online or in the room from MSF, Vietnam, Haiti, Australia, Bangladesh, Sudan and Scotland (yours truly).
We are beginning to link more about NCD support with colleagues in Gaza, the Ministry of Health and in WHO. However, without a ceasefire the risk remains high for everyone and the ability to offer support is so limited. Oral morphine access is very complicated, but we hear so many stories of terrible pain and suffering which is heartbreaking and demoralising for staff, that we are keeping looking for ways to bridge this gap.
(Dr Mhoira Leng has since travelled with a Canadian team to explore these issues further and offer some clinical support, but most of all solidarity and presence. Another blog will be posted with further updates.)
The last few weeks have been special for Muslims with Ramadan and for Christians with Easter. As we consider the time with its usual celebration, listen to what Suha, our wonderful oncology and palliative care pharmacist says.
“Like these days in previous years, we were racing to receive Ramadan with decorations, lanterns, and preparing Suhoor and Iftar menus throughout the month.
The streets of Khanyounis were full of people, decorations, crowds, and sounds of Ramadan welcoming songs.
Ramadan comes this year and we can't receive it in what befits it.”
The niece of Dr Amjad adds this,
“We just wanted the most beautiful month of the year to come while we were in our homes preparing for it at this time. Five months … and our hopes, hearts, dreams, wishes, and finally our future are still destroyed. Thank you, world.”
Please continue to keep informed, be involved in any way you can, and pray. Here is a beautiful prayer from Professor Alison Phipps and a reply from her Gaza colleagues:
Bless the helplessness
Bless the utter helplessness
Bless the unutterable agony of utter helplessness
Bless the endlessness of the helplessness
Of a helplessness that still resists death daily
Even as the helpless are dying for want of help
With the reply from Akram Sobhi Habeeb:
Bless the help that never ends,
Bless the endlessness of our friends
Bless those who defy despair by planting hope,
Bless the despair that ends with a strong rope,
Bless those who pray for the end of the war,
Bless those who keeps trying to open for us the door,
Bless those who keep praying for our cute kids,
Bless those who keep trying to make us well fed!
If you wish to donate to Cairdeas, then we are able to direct this to areas most in need.

Snapshot of Dr Mhoira Leng speaking on behalf of IAHPC at the WHO 154th Executive Board.

Sharing voices and the need to consider NCDs in humanitarian settings and emergencies.

After spending February in India, Dr Mhoira Leng sits with colleagues from Uganda at the first WHO High Level Meeting on Non-Communicable Diseases in Humanitarian Emergencies in Copenhagen.

Skies bright with hope in Copenhagen.

A pleasure to see fellow colleagues in the humanitarian settings; Dr Rachel Coghlan and Dr James Smith.
