
World Hospice and Palliative Care Day in Kampala, Uganda
![]() Hannah Ikong
Hannah Ikong
![]() 10th November 2022
10th November 2022
With twenty-nine years of palliative care services in Uganda, World Hospice and Palliative Care Day (and the week leading up to it) was something to celebrate.
One notable event was a public lecture on palliative care, which was organised by the Ministry of Health (MOH) plus the Palliative Care Association of Uganda (PCAU) and facilitated at the Davis Lecture Hall (Makerere College of Health Sciences, Mulago Hospital). It was encouraging to see so many students and healthcare professionals, as well as the online attendees on Zoom, on the afternoon of Wednesday, 5th October.
The team of Mulago Palliative Care Unit (MPCU)/Palliative care Education and Research Consortium (PcERC) was actively engaged in the public lecture. The team managed the registration table and handed out brochures and drinks. Both the team working in Kiruddu and Mulago Hospitals came for the event and were very proud to see their own Dr Liz Namukwaya present about the unit and sit in the Q&A panel.
Dr Liz Namukwaya spoke on the unit’s clinical activities, role in education, and extent of research. With an estimated 46% of patients admitted needing palliative care, the palliative unit alongside LINK nurses has served 12,520 patients since 2008. The unit has also trained over 3,500 students, from postgraduate and undergraduate doctors, nurses, pharmacists, to social workers.
Several other doctors presented on palliative care; first, Dr Fredrick Nelson Nakwagala, the Clinical Head Directorate of Internal Medicine at Mulago Hospital, talked about non-malignant conditions requiring palliative care. He shared stories of breaking bad news and encouraged fellow healthcare professionals to see the patient as a person, not as their illness. Dr Peter Lwabi, the Deputy Executive Director of the Uganda Heart Institute, then addressed the interdisciplinary approach of palliative care and cardiology.
The keynote speaker Dr David Okello presented on community engagement for alleviating pain and suffering in palliative care patients. As the Executive Director at African Center for Global Health and Social Transformation, he shared about the effectiveness of community involvement in COVID-19 and how the community contributes to holistic care.
The public lecture availed to much discussion among the Q&A panel and several remarks from palliative care leaders in attendance. The questions from the audience had to be cut short due to time, yet many were requesting for palliative care refresher trainings. Dr Anne Merriman, founder of Hospice Africa Uganda (HAU), gave some of the closing remarks as she reminded us to take care of the carers; that is, amid all the clinical activities, training, and research, we ought to care for ourselves and our colleagues.
World Hospice and Palliative Care Day (WHPCD) then was on Saturday, 8th October. The theme for this year was “Healing Hearts & Communities” which aligned well to the messages shared in the public lecture.
The palliative care unit of MPCU/PCERC was actively involved in the day’s events from the National Palliative Care Walk in the morning to the PCAU Palliative Care Fraternity football match. The unit contributed to the sponsorship of the day and assisted with the organisation, and they were glad to meet others who worked in palliative care across Uganda. The walk was about 4 km long, which started in the Mulago field/playground to Kamwokya (around Acacia Mall) and back again.
Liz Nabirye, the Clinical Lead of PcERC, noted that “it was a good health exercise and the first time to celebrate together since COVID. Later back at Mulago, we had speeches were made from the director of PCAU [Mark Mwesiga] and each palliative care organisation had time to talk about what they do.” She specifically recalls meeting other units from Masaka in western Uganda as well as Jinja (east-central), and they were able to share what services they offer and how they could refer patients to each other. “It was a unifying celebration for us, it was a palliative care fraternity,” Liz concluded.
This day of advocacy and awareness to palliative care was true to its theme, and healing hearts and the community involved a bit of fun! The team had practiced for weeks for this, and how it was finally here: a football match of representatives of the palliative care fraternity against members of the Ugandan Parliament. The two representatives from PcERC, Toko Friday and Bemustar, played well and tried their best. But in the end the parliamentarians wone the match, 6-3.
Nevertheless, PcERC was awarded a certificate of participation, and the team brought many good memories and new contacts from the day. “For me as the lead,” Liz Nabirye told me, “I would just say being a part of the events was a good thing to happen to our unit; we were able to create awareness, be represented, and be involved in the preparations. The week was for our advocacy … it raised visibility for palliative care services at the national referral hospitals.”

The official advertisement for the World Hospice & Palliative Care Public Lecture hosted by the Ministry of Health and the Palliative Care Association of Uganda.

A member of the audience inquiries the panel about how to encourage colleagues in their treatment of patients suffering and in pain.

The panel in person and on Zoom; questions kept coming in from both audiences! Pictured from left to right: Dr David Okello, Dr Fredrick Nelson Nakwagala, Dr Liz Namukwaya, and Dr Peter Lwabi.

Final remarks from Dr Anne Merriman of Hospice Africa Uganda: “Care for the carers.”
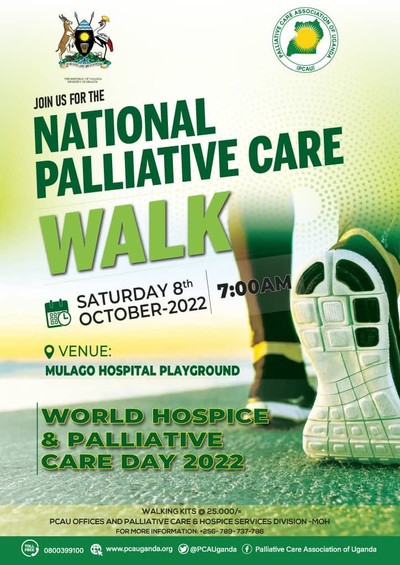
Official invitation to the walk sponsored by the Ministry of Health and the Palliative Care Association of Uganda.

The team from PcERC watching the football match; left to right, Liz Nabirye, Josephine Kabahweza, Vicky Jeminah, and Ronald Mukasa.

Our football player Toko Friday Santiago takes a quick break and stands near the team.

The certificate of participation to PcERC for World Hospice and Palliative Care Day and Week.
Photovoice and Palliative Care: Expanding Research in Adjumani and Obongi
![]() Hannah Ikong
Hannah Ikong
![]() 10th November 2022
10th November 2022
We are eager to incorporate Photovoice into the Transform Project in the Adjumani and Obongi districts of Uganda. Photovoice adds a deeper layer to the current data collection, helping us to better understand the lived experiences of severe health-related suffering (SHS) whilst staying in fragile communities. Photovoice is rather new in palliative care research in Africa, but on 22nd August we were able to receive a refresher training from Dr Jane Bates who utilised Photovoice with patients and their families and caregivers in Malawi.
What is Photovoice exactly? Perhaps we can first tell you what it is not: Photovoice is not when a medical researcher visits a new area, evaluates a patient while taking pictures of the setting, then shares a story of what they found. Rather Photovoice is a dialogue where the patients (and/or families and caregivers) use photography to express themselves and share what is most important to them. Photovoice is a great addition to advocacy and self-representation, for it allows the community to speak for themselves by removing the newcomer’s perspective in the storytelling. Dr Jane Bates includes the three goals of Photovoice in her article, Enhanced patient research participation: a Photovoice study in Blantyre Malawi:
1. To enable people to record and reflect their communities’ strengths and concerns.
2. To promote critical dialogue and knowledge about important issues through large and small group discussion of photographs.
3. To reach policymakers.
During the refresher training, Dr Jane Bates spoke about her experiences of using Photovoice among patients with palliative care needs and their families and caregivers. As palliative care, in itself, has a patient-centred approach, it was thought best to use this participatory method of research, allowing those being ‘researched’ in Malawi to become the ‘researcher.’ Conducting the study at a community-based palliative clinic, they recruited six patients and seven carers as co-researchers during a period of four months. Their co-researchers were given digital cameras and through some nine group sessions, they took pictures, selected, and analysed their printed photos, later captioning a few of them in their own words. This process was reported to aid in open dialogue and, at times, assist in clinical review. The third goal of reaching policymakers through Photovoice was achieved at the end of study when they held a photo exhibition and advocacy event, which was attended by the local leaders and media.
Dr Jane Bates also discussed some cautions or concerns raised from their Photovoice study. For instance, this method of research excluded some patients with severe palliative care needs who could either not attend the sessions or see the pictures well. For others who were able to work, the structure of the group meetings was a challenge and they ended up missing some sessions as they needed to work and provide for themselves.
She challenged the leaders of the Transform Project to consider how we could bring Photovoice to Adjamani and Obongi districts, and how we could accommodate those who are more seriously ill and those who need time to work and make a livelihood. We then discussed our proposed research structure that may mitigate these challenges. For one, the trained Village Health Team members (VHTs) carry a smartphone with a camera, so they would work with the patients and their families individually to take photos, select and analyse them. VHTs also do travel to a patient’s home, giving those who are immobile an opportunity to participate and have a voice. Ideally, our VHTs could also liaise with those who are working outside the home and find times to meet and share in the Photovoice research.
It is clear to the Transform Project leaders that Photovoice is a necessary addition in our data collection. We already have the backbone needed for this participatory research method; the VHTs hold smartphones and have been trained how to use the camera, we have a network of patients, families and other caregivers visited regularly by the VHTs, and now our leadership team has been trained in Photovoice methods and the process. The next step will be sharing what we have learned with the VHTs so they can begin the Photovoice process.
Liz Nabirye, clinical lead of PcERC and a part of the Transform leadership found the training applicable to more than just our research in Adjumani and Obongi districts. “To me,” she said, “it is not just a methodology to use for this project, but to train our volunteers in the Kampala Hospitals to learn to use Photovoice and engage with our patients and our families. Photovoice is a strong method of getting quality, important information … [we can] work with the patients and their families and make meaning of the photos and what they are communicating to us.” We thank Dr Jane Bates for the invaluable mentorship she has given the team by sharing her own experiences and advising us in integrating Photovoice to our current research. Do stay tuned for more Photovoice updates, coming soon from Uganda!

Transform Project leaders pose for a photo with Dr Jane Bates. Pictured from left to right: Dr Mhoira Leng, Toko Friday Santiago, Immaculate Atim, Dr Jane Bates, Liz Nabirye, Dr Liz Namukwaya, and Godfrey Oziti.

Selfie time with the author of this blog, Hannah Ikong.
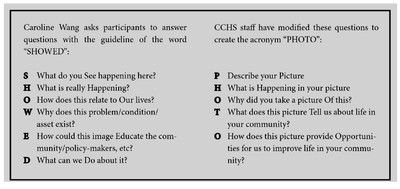
Discussion questions for Photovoice dialogue shared by Dr Jane Bates. We walked through each question and even participated in role plays to see how “SHOWED” and “PHOTO” questions could facilitate deeper discussions.
Compassion and Dignity are Cornerstones of Palliative Care
![]() Hannah Ikong
Hannah Ikong
![]() 4th November 2022
4th November 2022
Intitally shared on the AIDEM, 10th October 2022: On the eve of World Mental Health Day, Dr. Chitra Venkateswaran, Psycho-Oncologist and Clinical Director of Mehac Foundation, interviews Dr. Mhoira E.F. Leng, a renowned international palliative care expert from the United Kingdom. Dr. Mhoira has been instrumental in coordinating pain and palliative care work across the globe. Her vision of palliative care encompasses the values of compassion, dignity, hope, and community involvement.
Highlights from the interview:
[Regarding palliative care]: “we recognize that it's something that needs to be connected deeply, to individuals; individuals affected by palliative care need, individuals who are offering palliative care need, but actually, they together form communities. And if we can connect with meaning, and hope, and values, and what we're going to say about the most marginalized in our communities, to our core humanity, then I think palliative care begins to make sense. If we see it simply as a medical specialty, it stays in the hospital setting and the medical setting.” – Dr Mhoira Leng
“We have a role as a doctor as, as medical professionals, as healthcare professionals, to take care of people who need palliative care. That is probably one of the most important sections of palliative care. But I believe that palliative care as a philosophy has much more relevance in the dimensions of people's lives or in communities.” – Dr Chitra Venkateswaran
“At the core of everything we do are our values, and the values that are distilled out in palliative care, because it deals with such crucial issues such crucial times in our lives, it makes us reflect on and maybe even challenge and develop our values. And I think we've seen this in these last few years with the pressures of a pandemic. We've seen it in Kerala [India] with the floods, and the pressures and challenges that came from that, and different parts of the world different ways. But it brings us back to what's important, what gives our life meaning.” – Dr Mhoira Leng
“Access to medicines like morphine as painkiller [are] absolutely vital. But why is it vital? It's so that when we have our pain controlled, we can have those conversations with our loved ones, we can make the decisions we want to make for our families. And I think it's that transformational ability that palliative care has. And there's one value I think we talk about a lot: compassion, yes. There's … an equation, people are talking about at the moment that compassion is awareness, plus empathy, plus action. And that equals compassion. And I think that's something that we see in the journey of palliative care.” – Dr Mhoira Leng
“That sense of being there for people, even when you don't have all the answers … and you're walking alongside that presence and holding that presence. Again, you can describe it almost like a candle, and you're holding those places between fear and doubt and hope and despair, those you're holding those places, not necessarily with all the answers, but saying ‘we are there,’ ‘we are going to do all we can to improve the quality of what's happening for you.’ But most of all, ‘we won’t abandon you.’ – Dr Mhoira Leng
“I think that [there is a] balance between all these domains, you know; having a good symptom control, taking care of all the physical symptoms that a person has, but as well as looking into all those spiritual, these emotional aspects, the mental health issues, which again, came up really visibly, you know, noted during the COVID pandemic. I mean, we saw so much of a surge of mental health issues. We saw, you know, the grief that came in; the cumulative grief due to the losses.” – Dr Chitra Venkateswaran
“We're seeing it in different ways, where we are kind of defining ourselves by who we are and who somebody else is not. You know, we're increasingly defining ourselves, we're this and you're this. And I think what palliative care teaches us isn't the end of the day do these things matter? They don't. What matters is me as a human being connecting to you as a human being, at times in our lives, which are, are some of the most meaningful, the most difficult, but also the most precious. So I think more than ever, we should say to societies and settings, what is it that unites us? … perhaps palliative care brings us right back to that. It's about our common suffering, or common humanity and the compassion that we, we as individuals, but we as societies, and we as a global community, and need to remember, discover, celebrate, [and] develop to respond to the need.” – Dr Mhoira Leng
“If we just take end of life care: it's such a precious time, it's the last time we spend with loved ones. It's such an important time to make sure that things like pain is controlled, that people are not distressed … there's everything we can do, to support families, to support the process. So that, that, that can be as meaningful and gracious as possible so that the loved ones can hold their hand and be there together, they can say the things that are important to them. That things like saying, ‘I'm sorry,’ reconnecting, building relationships, seeing priorities can happen. And perhaps we need to bring that into our conversations.” – Dr Mhoira Leng
“The clinical or the, the medical fraternity also perceives death as a failure. Isn't it like, when somebody dies, someone with a chronic illness (or even any illness dies), they perceive it as their own failure to cure them, because cure is the ultimate success. So to gently let go, you know, for the physicians or for the medical professionals, as well, to know when to stop …” – Dr Chitra Venkateswaran
“When we talk about clinicians, you know, changing their perspective about how to manage, I think the start should be also discussion about death openly in the society. And I have seen it, there's been a lot of efforts from colleagues and friends across India, they, they have these death cafes, where people talk about it talk about death and dying in a much more open way. Because we usually do not—that is a taboo word isn’t it—you do not talk about that. It's as if that it has not happened to me, it happens to somebody else.” – Dr Chitra Venkateswaran
“Palliative care allows us to move back again. Maybe countries like India, or many other countries in Africa, and Palestine can teach also about what it means to be a collectivist, absolutely collectivist community orientated. But still, we need to make sure we're discussing life and death and all its glory, and its joys, and also its pains and its challenges. So I think it's important to also remember that palliative care and being human is something that brings laughter and joy, as well as tears and sorrow—and it's that whole package that makes us human.” – Dr Mhoira Leng
Feedback from the interview:
“Dr. Chitra and Dr. Mhoira,
It was really an excellent conversation. Really everyone needs to listen to this, within a short time what is palliative is clear. Hats off to both of you.
Watched the whole interview.”
– Stella Alice Verginia
“Great to hear such a comprehensive, global, yet relatable aspects of Palliative Care from Mhoira. Thank you for that.
Excellent conversation Dr. Chitra. You should do this more often.”
– Dr Biju Rhagavan
“Beautiful, explained the profound philosophy of palliative care.
Congrats Mhoira and Chitra.”
– Dr Geetha Vijay
“Mhoira, I just listened to your excellent talk with Chitra about compassion & dignity. I found myself taking notes again!
I loved your expansion of ‘compassion’. Many in my circle had awareness but lacked empathy & action.
Thank you for your Gaza stories, a situation that distresses me greatly.”
– Dr Ann Thyle

