
100 hours in India: Palliative Care, Nephrology, and the best Parathas
![]() Hannah Ikong
Hannah Ikong
![]() 27th March 2023
27th March 2023
What can you accomplish during a little over four days in India? For Dr Peace Bagasha, there was quite a lot to do.
Peace is a renal specialist working at Mulago Hospital who is pursuing her PhD via research at Makerere University in Kampala, Uganda, In the short time between 9th and 13th February, Peace retold her many trip activities and palliative care sessions to the Cairdeas communications team. It was a lovely, jam-packed 100 hours, she reports, yet not nearly enough time to read the book she brought!
Peace’s short journey began in Bangalore where the Indian Association of Palliative Care (IAPC) held its 30th Annual Conference, #IAPCON2023. This conference was not your typical palliative care get together. First, for Peace, her time there was more like an annual palliative care family reunion.
Joining other palliative care specialists like Dr Mhoira Leng, Prof Julia Downing, and Dr Chitra Venkateswaran, they attended a dinner on her first night there, with other presenters and organisers of IAPCON 2023. As many at Cairdeas may know, Mhoira has been a part of this IAPC conference since its beginning, and so it was a pleasure to catch up with old friends.
#IAPCON2023 was also unique in the theme and set up of subspeciality tracks. This year’s theme was “Metamorphosis: The Emergence of Subspeciality Palliative Medicine” and Peace explained how the conference sessions were designed to bring out each subspeciality and demonstrate the role palliative care in it.
For Peace herself, she presented for 30 minutes on nephrology and palliative care, or “renal supportive care.” Her presentation title was, “What is the evidence HRQoL, survival benefits of patients with ESKD receiving Haemodialysis, Vs. Conservative Kidney Management.”
Peace shared about the other tracks she attended, such as a session in cardiology titled “Role of nurses in managing heart failure.” The speaker, Sister Hanife, advocated nurse empowerment, which implicates nurse inclusion in patient decision making. Hanife argued that nurses are involved in so much hands-on care, and we need to appreciate their experience and support in caring for patients, especially at end of life.
While Peace spent most of her time at the conference while in Bangalore, she had several highlights of the area itself. Bangalore was a “garden city” and the beautiful greenspaces were enhanced by the good, cool weather while she was there.
She then shared about Karunashraya Hospice, which hosted the dinner on their first night there. Not only is the hospice facility beautiful with gardens and ponds, but they are the first hospice in India to provide free home-care for terminally ill cancer patients. Their website explains more, saying, “Since the launch of home care services in 1994, we have cared for more than 3000 patients, and have around 50+ patients under our care at any point of time.”
I had to ask Peace about the delicious types of food she ate while on her trip in India. Her answer surprised me: Paratha! Like the flat chapatis you can find in Uganda, another partner country of Cairdeas, Parathas are unleavened Indian flatbreads made with whole wheat flour. I asked Peace if she only ate this tasty bread, and she laughed. “No,” she said, explaining that you can eat with curries like chicken or lamb.
You may think the 100-hour journey stops here but there is was one more trip: after her presentation at #IAPCON2023, Peace travelled to Mumbai and some managed to participate in a workshop, tour some of Mumbai, and visit a hospital paediatric palliative care unit.
We spoke mostly on her workshop that she engaged in about renal supportive care. The workshop had several rich discussions, she said, since many nephrology groups are starting to integrate palliative care into their programmes.
The workshop was a good learning environment too, causing Peace to conclude, that for her place of work in Uganda, “I think we really need to set up a really structured renal supportive care programme.”
How would you spend a short 4 days in India? In a little under 100 hours, in short, for Peace, she was presenting at a conference and participating in a workshop, touring the area,and visiting a hospice and a hospital, all spanning two beautiful and diverse cities. Reading that sentence can leave you a little breathless!
Even so, we wish to extend a very large thank you to Dr Peace Bagasha for her work and role in renal supportive care and for #BuildingaWorldthatCares.

A lovely picture of Prof Julia Downing with Drs Peace Bagasha and Mhoira Leng.

Dr Peace Bagasha at Karunashraya Hospice.

Dr Peace Bagasha points at her session at the IAPCON conference: “What is the evidence HRQoL, survival benefits of patients with ESKD receiving Haemodialysis, Vs. Conservative Kidney Management.”

A group photo while in Bangalore: Drs Peace Bagasha, Ann Thyle and Sid, Prof Chitra Venkateswaran and Dr Mhoira Leng.

A traditional dance performance at the conference! What would you do if you had 100 hours in India?
Integrating Palliative Care in Fragile Settings: a Transformative Paradigm
![]() Hannah Ikong
Hannah Ikong
![]() 10th March 2023
10th March 2023
We're pleased to share a webinar on "Palliative care in low resource and fragile settings" from Dr Mhoira Leng, given on 23rd February 2023 and hosted by the International Christian Medical and Dental Association (ICMDA).
The talk was introduced as this: "Compassionate care for the whole person is at the heart of palliative care. Walking alongside people and their families facing chronic illness and into the end of their lives is an immense privilege. In many parts of the world this care is not available representing one of the greatest health inequalities. In other situations, economic, cultural and political pressures can undermine values orientated, faith based holistic care. In Jesus we have the ultimate example of compassionate holistic care... how do we reflect his example in how we approach suffering and how we care for those those in pain?"
I would encourage you to watch the video recording to explore the answers to this question from the talk and the discussion that followed. Below I have included some of my own highlights of the webinar, all quotes from Dr Mhoira Leng.
Excerpts from the webinar:
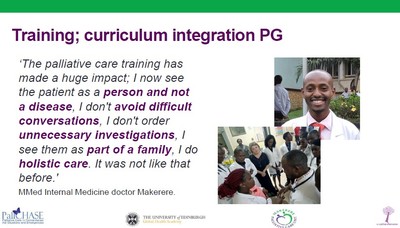
When I want to talk about transformation today, I want to come to the heart of palliative care, holistic care for people living with chronic illnesses which includes the quality of life of that living, but also the quality of life of the end. The end, the dying time, is a very precious and important time, but not the whole of palliative care, and on to supporting families and bereavement.
I want to think about this transformational model in lives, in practises, in systems, and in societies. What is at the core? Values based holistic care, promoting dignity … the relief of suffering, demonstration of compassion, not just the empathy, but the demonstration of compassion. And alongside that, for me, particularly when I think of the inequalities of our world (and I am going to say something about those) fighting for justice.
[In reference to the integrating palliative care house diagram, with people at the centre.] The patients and their families are at the heart of this. There's a number of very helpful indicators that you can look at if you are setting up services or want to know more. I would encourage you to do that [follow indicators], but doesn't make sense for this gentleman, an amazing man I met in the refugee camps in the north of Uganda, and where we've been doing some work. He was telling me how they built a 1,000-seater mud hut church. His request for me was, “Can you find us some Bibles in the Bari language?” So the needs may not be the ones that we expect, but we need to be able to listen, and it needs to make sense for a gentleman like this.
Just one last thought in terms of looking at this global picture. This is the floods in Pakistan, and we're looking at the earthquakes in Turkey and Syria. We're hearing of storms even now of Madagascar and Mozambique. Planetary change, climate change, is disproportionately going to affect those who are not already fragile, and that as that must be part of our thinking and part of our Christian response.
There is a term called fragile settings. If you're not aware of it again, you can have a look at the detail of this, but it's a way to understand, not just the places where this active conflict or in natural disaster, but the countries, next door those where there is political instability, or weak health systems, or a high burden of disease, or protracted emergencies. And I think you look at this map, and you're not surprised to see many countries in Africa, but also in the Middle East and Afghanistan … So what is palliative care mean in those settings?
There's a word which my Gaza students use when we're talking about spiritual distress. It's an Arabic word which says, our world has been shaken. And I think for me that represents the distress that is the heart of suffering, and much of that distress will be spiritual. Of course we talk about the financial, the social, the physical, the emotional, but at the heart of much of the distress is that lack of meaning and open purpose. What do we say to people whose world has been shaken? Or how do we respond to people?
One of the values of quality [palliative care] is compassion. And this is not a lovely acknowledgement of the role that we have in bringing compression into these settings. Let me just give you some specifics. … In Malawi, Jane Bates has a wonderful paper which talks about how making better choices, giving people information, helping and giving support them at home, may, in fact, reduce poverty. This is really important in our fragile settings, so that people are making the right decisions for them.
I’ll just finish by asking you what gives you hope? How do you restore your hope when you're engaging in suffering? Some of the things we talk about when we talk about hope, and breaking bad news, and tender conversations; meaning and connection and comfort and love and hope and presence and strength. And ultimately we find that in that deep relationship with the loving God who has forgiven us, who has saved us, and has given us ability to have a relationship with us and the privilege of working in his purposes and plans.
This is one hope that I love and I think of often when I'm walking that journey with people. God shall wipe away all tears from their eyes, and they shall be no more death, neither sorrow nor crying, neither there shall be any more pain, for the former things passed away.
Snap of Dr Mhoira Leng during the webinar. Fun fact: she recorded this talk while in India!
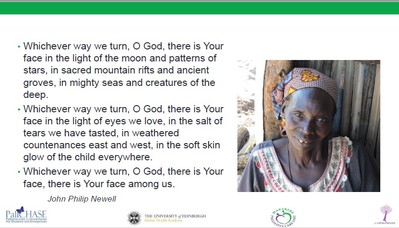
Opening prayer and reflection to the presentation, ending with: "Whichever way we turn, O God, there is Your face, there is Your face among us."

Using the photo of a chrysalis turning into a butterfly, we see transformational change from palliative care in lives, practice, systems, and societies.
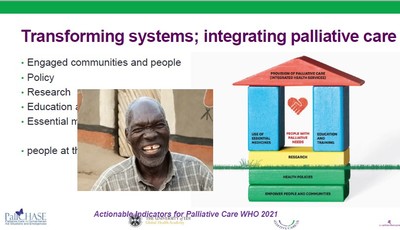
Actionable Indicators for Palliative Care (WHO 21) build a home of support around the patient and family. Pictured is a gentleman whose surprising request for Bibles reminds us to ask and then listen.
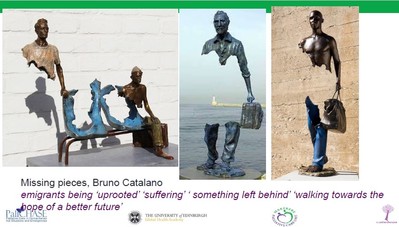
There are many graphs and charts that describe fragile settings where palliative care is needed the most. These sculptures by Bruno Catalano speak even deeper than the numbers of refugees.
There's an Arabic term that means "when our world has been shaken." Spiritual distress often feels like this.
Watch the video recording for more examples of transformative palliative care education and capacity building.
Finally, finding true hope and strength to better #BuildingAWorldThatCares.
Bringing Palliative Care to Psychologists and Social Workers in Sudan
![]() Cairdeas
Cairdeas
![]() 10th February 2023
10th February 2023
Blog submitted by Dr Nahla Gafer, a clinical oncologist at the Khartoum Oncology Hospital, Sudan. Dr Gafer has been involved in past regional training in palliative care, such as the Kuwait WHO PC workshop and in Mauritania through Cairdeas Sahara. Today she shares about her recent workshop for psychologists and social workers.
Let me start with the beginning of my palliative care journey: it was 2009, and for the first time, I attended a formal course in palliative care at Hospice Africa Uganda. I was intrigued by the weather, intrigued by the vegetation, and intrigued by the organization. I remember meeting Prof Anne Merriman in a beautiful summer house. And I remember seeing a coloured brochure describing items like a 5 week Initiators course, a 3 day workshop for psychologists, and 9 month programme for nurses. I was thrown out of my feet. How organized they are and how developed they are in palliative care!
Years pass, a palliative care unit is born with staff from Sudan are trained in palliative care. I go abroad to complete my Master’s degree in palliative care, and I advocate for palliative care. In this time, I meet SANAD Lebanese Association for Palliative Care and our team trains in a Hospice@Home programme. SANAD then organizes an online course for 27 health professionals, where several psychologists attend the workshop. The director of training at the Ministry of Health in Sudan contacts me about further training. And so, a three day palliative care workshop for psychologists and social workers is planned for and conducted end of 2022.
I am so glad that I was able to conduct this workshop. In the beginning I thought I could not elaborate much when it comes to items like symptom management as they are not doctors. Yet I discovered that when teaching palliative care, a lot can be explained even to non-health professionals, and especially for the candidates in this workshop, the majority of whom have long experiences in specialised hospitals.
Twenty-five psychologists and twenty-five social workers attended the workshop, representing 23 specialized hospitals as well as the Federal Ministry of Health. My job was easy, I just gave them a new outlook for the problem: the patient is the centre of our care, we are here to help the patient and family until the end by providing explanations, support, symptom management and a listening ear.
It was a wonderful experience for all. As an example, we came up with 50 activities for self-care, and as I mentioned even for symptom management I succeeded in explaining a lot: what symptoms to expect in which diseases, how to assess them, how to think holistically and how to manage those symptoms non pharmacologically. As for the pharmacological management, I asked them what medications we use, without elaborating on the doses, route, or timing.
We delved into family issues, attachment types, complicated grief, suicidal tendencies, distress, anxiety and depression. It was very interactive and very engaging. I was joined by nurse named Wafa Abdalla and a psychologist, Eman Mansour, who both came from our palliative care unit to assist me in the training.
The feedback after each session was great. Candidates mentioned that they learned important concepts like: patient’s dignity, patient’s rights, quality of life, taking into consideration patient's age, understanding and cultural background, the six steps involved in breaking bad news, instilling hope, different types of hope, the importance of explaining the disease to the patient and family, and most importantly that palliative care brings back humanity to the patient (i.e. patient feels he/she has a say in what is happening).
They felt palliative care aligns well with the needs of the patients they meet in their day-to-day work, and a couple of them were eager to contact their administration for training in their hospitals, with a subsequent plan to provide the services. I am open to help, and I am thankful for all my teachers in palliative care.

Dr Nahla Gefer (in yellow, second from the left) poses with candidates who attended the palliative care workshop.

Ms Mai Sabir, State Ministry of Health, Dr Nahla Gafer, Sr. Wafa Abdalla distributing certificates at the end of the 3 day workshop.

Dr Fayrouz M Abdalla from the WHO NCD office, congratulating the candidates.

End of the workshop group photo with certificates.
