
Mapping The Way Ahead – New Strategic Plan Launched
![]() Cairdeas
Cairdeas
![]() 11th October 2018
11th October 2018
Cairdeas is delighted to have amazing partners in Uganda who are forging ahead with plans for the next five years. The newly launched Palliative care Education and Research Consortium (PcERC) working through a partnership with the Makerere & Mulago Palliative Care Unit (MMPCU) have just launched their next five-year Strategic Plan. Mapping the way ahead for the period 2018-2023, the plan presents clear and achievable strategies under five thematic areas: Clinical Service Provision; Education; Research; Advocacy; and Sustainability. You can find a copy in the Resources section of our website under 'MMPCU and PcERC'
Exemplary patient care is the ultimate aim of good clinical service provision. Under this first theme, the plan describes how physical, social, psychological and spiritual needs will all be addressed in caring for patients. This will require integration and joined-up working within and across primary and hospital care teams. One patient said, “They talked to me, encouraged me, and helped me to get medication. The pain has become manageable. There was tremendous improvement. I did not feel like the way I was when they first found me.”
Strand two of the strategic plan, education, is concerned with providing education, training and capacity building for healthcare workers, allied health professionals and volunteers at all levels. PcERC is aligned with the education vision of MMPCU, Makerere University, and Uganda’s Ministry of Health, all of whom seek to integrate palliative care competences across health and social care curricula. The education strand of the strategic plan seeks to go further in ensuring palliative care is also mainstreamed into theology and community programmes. This change of approach has already affected many doctors and nurses for the better, with one saying, “Palliative care has made a huge impact: I now see the patient as a person and not a disease. I don't avoid difficult conversations. I see them as part of a family. I do holistic care. It was not like that before.”
The third element of the plan, research, seeks to continue to expand the evidence-base for palliative care by building on research collaborations within and outside palliative care service provision. Understanding what works best for the patient, what delivers best outcomes, must be underpinned by solid evidence. PcERC will continue to promote the research culture already prevalent amongst its partners, and seek to review, disseminate, and publish findings with a view to influencing and improving policy and practice. Speaking of their hunger to ask questions and find out more, one researcher said, “The training, whilst I was doing my Bachelors in palliative care, has helped me to continue with research, trying to find out: if I do this, then what?”
Advocacy to enhance and promote academic and clinical credibility for palliative care, is the fourth strand of the strategic plan. PcERC will seek to work in partnership to advocate for Universal Health Coverage, acting as a voice for those most vulnerable groups living with chronic illness such as: migrants and refugees; children and the elderly; those in need of legal support; and those affected by poverty. PcERC pledges to work collaboratively both in Uganda and internationally and to continue to advocate for those who are denied any or adequate palliative care treatment. A senior nursing colleague in Northern Uganda who is part of PcERC and Cairdeas partnership with Peace Hospice, Adjumani spoke of what she has seen through the work of palliative care: “Someone needs to speak for the voiceless. When help comes, people change, then hope appears suddenly like the sun.”
There is no decrease in the number of people requiring palliative care and so the final element of the strategic plan - sustainability - is essential in ensuring the continuing needs of patients are met. PcERC seeks to develop a well-resourced palliative care unit, with sufficient personnel and infrastructure capable of supporting a Ugandan-led palliative care programme into the future. This will require effective and responsible use of financial resources, good governance, and robust monitoring and evaluation systems. PcERC will also, where appropriate, seek to attract grants, consultancy projects, and partnerships that will add to its financial sustainability and growth.
Grace Kivumbi, a member of the Board of Directors for PcERC said,“I see this as an opportunity to grow and expand our services to other institutions were many patients are suffering in pain but without access to the much needed palliative care but also as a means towards sustainability of the service.”
Key to this is the establishment of sustainability and PcERC and MMPCU is working hard with University and MOH colleagues. However it is also seeks to develop a direct donor network. Would you like to be involved in directly supporting this work or to give to Cairdeas as we seek to strengthen partnerships and sustainability? Think about donating here.
MPCU senior advisor and PcERC chair, Dr. Mhoira Lengspoke of the “privilege it is to have been invited to lead developments of the past 10 years and now to see PcERC launched and moving forward. We are praying the current significant resource challenges have some movement and that the amazing MMPCU team can continue to grow, train, inspire and care for those in need.”


Warmth, Sympathy and Understanding: Dr M.R. Rajagopal visits Edinburgh
![]() Cairdeas
Cairdeas
![]() 11th October 2018
11th October 2018
Sometimes called ‘the father of palliative care in India’, Dr M.R. Rajagopal was in Edinburgh this week as guest of honour at a screening of a documentary on the achievements of his own extraordinary life. Entitled, "Hippocratic: 18 Experiments in Gently Shaking the World", it was hosted by EMMS International. The rapt audience, who had gathered in Royal College of Physicians, were soon to learn the truth of an introduction that described Dr. Raj as: “passionate, not timid; gentle, but effective.”
Originally from Kerala, in the south of India where he started his pioneering work, he is now the Chairman of one of the world’s largest networks of palliative care provision – Pallium India. Long time friend of Cairdeas, he has a close personal and working relationship with Cairdeas’ Medical Director, Dr. Mhoira Leng, and Cairdeas recently supported his visit to Uganda as the keynote speaker at their 10th anniversary conference.
Both his sincerity and passion are clear in everything he says and does. “Pain relief medication isthere,”he told us, “it’s just not getting to those who need it.”
He spoke openly and honestly about the significance of the Hippocratic Oath, and how its principles underpin and drive his work. He quoted elements of the oath verbatim, wrapping himself in its mantra of care and dedication:“I will remember that there is art to medicine as well as science, and that warmth, sympathy, and understanding may outweigh the surgeon's knife or the chemist's drug. Above all, I must not play at God.”
Without doubt, access to pain relief medication was highlighted as an enormous issue but so, he told us, was one’s attitude to serving their patients. “We have the power to destroy with a few words, or to lift up with a few words.” He guarded against the medical profession becoming trapped in their heads and detached from their hearts as he emphasised that the treatment of the person is as important as the treatment of the pain.
Again and again, he stressed how ‘good’ palliative care must treat the patient with care and respect, not simply treating them as a receptacle and ‘attacking’ a disease. Human beings, he told us, are much more than just containers of disease. In a room filled with doctors and nurses he reminded those present from the caring profession that they are in a position of ‘huge privilege’; but one that requires empathy, one that asks you to walk in the shoes of another, one that requires you to understand the suffering of fellow man.
Over the years Dr. Raj has drawn much inspiration from his fellow countryman, Mahatma Gandhi, whom he often quoted. “Recall the face of the poorest and weakest man you have seen, and ask yourself if this step you contemplate is going to be any use to him.” This line from Gandhi informs Dr. Raj’s decision making every time as he strives to serve those in the depths of poverty with nothing; a poverty, he told us, which Gandhi called, “the worst form of violence.”
Towards the end of the film, Dr. Raj said very simply: “When I started to work in palliative care, I started to learn about life.” If you ever need a reminder as to why you are working in palliative care, or why you are supporting the work of those delivering palliative care, please get your hands on this film and watch it. It will teach you so much about life.

Dr M.R. Rajagopal, Chairman, Pallium India; Eimear Bush, Operations Director Cairdeas IPCT; Dr. Amy Hardie, Director, Scottish Documentary Institute

Dr. Mhoira Leng of Cairdeas and Dr. M.R. Rajagopal of Pallium India, pictured a few years back in India
Shaping Palliative Care Work Globally
![]() Cairdeas
Cairdeas
![]() 3rd September 2018
3rd September 2018
Day two (10thAugust 2018) of Cairdeas and the Makerere & Mulago Palliative Care Unit’s (MMPCU) 10thanniversary conference was opened by Professor Liz Grant, from the University of Edinburgh. She began the day by highlighting how partnership work in Kampala has influenced, contributed to, and shaped palliative care globally. Prof. Liz framed palliative care in the context of the Sustainable Development Goals(SDGs); that collection of 17 global goals established and agreed by the United Nations Development Programme. She argued that good models of palliative care – such as those being pioneered by Cairdeas and MMPCU - help achieve SDG number three: Good health and wellbeing for people. Dr Grant also suggested that good practice within palliative care is replicable acrosswider health systems, and that the palliative care model in Uganda is an excellent response to the call for universal health care.
Dr. Jackson Amone then described the journey of palliative care for those with a serious or life limiting illness. He made clear the importance of a palliative approach throughout the course of an illness, but did not skirt the issue of the significant gap, globally, between the need and the availability of palliative care services. Dr Amone commended Uganda’s Ministry of Health in its commitment to ensure a consistent and reliable supply of free patient morphine.
Ensuring that the right care is available in the right place and at the right time, were elements of a conundrum explored by Dr. Sam Guma. He stressed the importance of continuum of care and explored factors that affect the delivery of a quality service, including timely referrals and the availability of services.
A discussion on the importance of the spiritual component of palliative care was led by Ivan Odiit Onapito. Ivan described a study that was undertaken with patients in Mulago Hospital to identify their feelings from diagnosis to treatment. The study raised several key themes including the importance of listening to the patient and the value of being present. Ultimately, it made clear the enormous value to be had in listening to patients’ stories. He concluded that spiritual support is an essential part of palliative care and he made a strong recommendation for ongoing mentorship for spiritual providers in palliative care to help them become better versed and equipped in the palliative approach.
A number of speakers delivered papers on palliative care in relation to specific diseases: Palliative care in end stage renal disease (Dr Peace Bagasha); Integration of palliative care into standard oncology (Dr Henry Ddungu); and Experiences of patients living with heart failure (Dr Elizabeth Namukwaya). Each concluded that holistic care is essential, and presented evidence that integrating palliative care results in improved outcomes across the board.
The practice of integrating palliative care was described Dr Nahla Gafer in a set of cases she presented from her work in Sudan. She highlighted how her work is bolstered by an effective programme of training and the partnerships with CairdeasIPCT, MPCU and University of Edinburgh.
Palliative care and mental health, palliative care and refugees, and palliative care and the elderly were three thematic areas addressed respectively by Professor Chitra Ventkateswaran, Vicky Opia, and Dr. Harriet Nankabirwa. In each presentation, compelling arguments were made to: address the mental health burden evident in palliative care; integrate palliative care into humanitarian emergencies; provide comprehensive geriatric assessment for older patients needing palliative care.
MPCU senior advisor and PcERC chair, Dr. Mhoira Leng, lent her full support to Dr Marcia Glass’s call to continue to establish, strengthen and build on the opportunities emerging from the many partnerships that are in place and have been cemented as a result of the conference.
“What a privilege to share the work of MPCU and our partners. It is exciting to see all that has been achieved but particularly to hear from those affected by chronic illness such as Helen. We need to be a voice for the voiceless and ensure we offer care with compassion and quality. As we launch the Palliative care Education and Research Consortium (PcERC) we move forward with the vision of palliative care for all.”
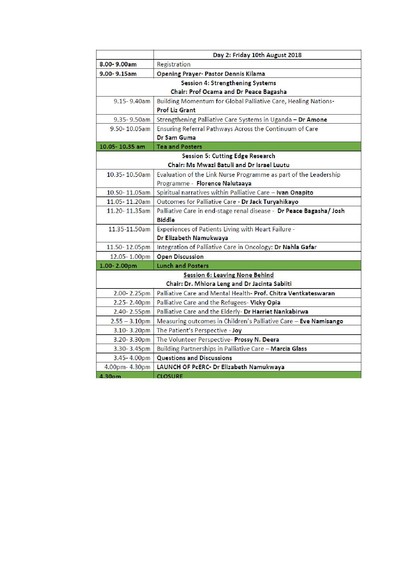
Day Two Running Order of Cairdeas and MMPCU's 10th anniversary conference

Sanyo team from Lugogo Baptist Church: 'Bringing joy, bringing hope.'

Dr. Peace Bagasha with ACN, Beatrice Amuge, chairing.

Naha Gafer bringing her pioneering work in Sudan to focus.

Long term friend and partner for Cairdeas International Palliative Care Trust, Chitra Venkateswaran, sharing her passion for those living with mental health problems and the model of MEHAC.
