
Cairdeas Scholars: Updates at end of 2023!
![]() Hannah Ikong
Hannah Ikong
![]() 16th November 2023
16th November 2023
Cairdeas International Palliative Care Trust is pleased to offer scholarships to partnering individuals and we currently have four Cairdeas Scholars. Hear more about each of their progress and their update below!
Godfrey Oziti
Studying a Diploma of Nursing in Gulu, Uganda
I am so delighted to talk and share some updates on my school! I am in the second semester of nursing and passed all my classes well last semester. In this semester, there are several topics to cover and papers to write and one of the topics is palliative care. We have also been covering community-based healthcare, primary healthcare, disaster management, and some occupational healthcare. Four of the papers that I have been writing are based on these theories, and the last paper is practical. It’s been wonderful to formally study palliative care, to better understand it as a whole and add to what Vicky Opia has taught me at Peace Hospice Adjumani.
Much of our palliative care course contains what we taught to the Village Health Teams, the VHTs: kinds of chronic, serious illness, holistic care, pain and symptom management, and communication like breaking bad news. I led my group members in being able to assess pain. One of the core palliative care instructors is a preacher as well, and he has taught me about assessing and addressing spiritual concerns in end of life. He gives us many “real life” examples in his teaching and has helped me better understand the role of spirituality in palliative care.
So really, I am really, really excited to be in this nursing programme; to go to school and gain knowledge. The knowledge that I am adding on now, is what I will bring to the community. I want to give special regards to Cairdeas IPCT for this scholarship. And after the end of this semester, by the second week of December, I will be going back and working at Peace Hospice Adjumani during the holidays.
Phillip Amol Kuol
Studying a Bachelor of Social Work in Arua, Uganda
Since our last communication, I have completed the Diploma course for social work and administration, and so I am now in my first semester as a Bachelor’s student. Let me explain quickly: for students without any diploma, their Bachelor degree would be three years, but since I was able to study for the Diploma with a Cairdeas Scholarship, I am halfway through the Bachelor’s degree. Now that it has been some time after COVID-19, the university is no longer offering online classes. I now live in Arua and attend all my classes in person.
In my classes, I am finding that some of the examples given where social workers are needed touch me personally. Either in my own experiences or experiences in the community; these familiar textbook examples remind me that I am part of humanity and also makes me remember my life in South Sudan. Social workers are needed for so many South Sudanese people; due to the war there, we now have so many different crises, suffering and abuse in our community [including refugee settlement camps]. Social work also addresses and touches the way people behave, including how we are brought up and what influences us to live certain lifestyles. I see the effects of war in our communities from issues like bankruptcy, cattle stealing, and domestic violence.
The way that the Cairdeas team has supported me makes me want to support others. It began when I was in Nyamunzi Camp in Adjumani, supporting clients with chronic illnesses and working with Vicky Opia, Dr Mhoira Leng, and Godfrey Oziti in palliative care. Helping others also has led me to join an organisation this year, a community-based organisation (CBO) called Dongriin Foundation which has the main activities of supporting education and providing mentorship to the youth in refugee camps. And so that is why I continue to say that the way Cairdeas has supported me, I want to support others; through providing guidance, mentorship, books and when possible, with finances.
Toko Friday Santiago
Studying a Masters of Social Work in Kampala, Uganda
How are my studies? I am doing well, I passed my first semester and now I am in the second semester. School is really about hard work and reading hard, and it has helped me grow in my knowledge base of social work and has given me some skills. An example is with the monthly social work reports I write for PcERC; I’ve discovered a more efficient way to report our social work activities from my classes.
Currently, my studies have given me some input on how to approach children on the ward [both paediatric patients and young family members] and one item of interest to me is play therapy. Another area of interest is advocacy in social work and how to support human rights. I am very interested in advocacy and would like to find more opportunities to do so in the team. I feel like in my undergraduate studies in social work, everything was so compressed in our syllabus, but with my Masters, I have been able to explore and go deeper in class.
The PcERC team has been helpful and flexible with giving me times of study leave, as well as time to go complete my exams. I have been able to balance work and school. I am grateful to Cairdeas for the scholarship and this opportunity to study social work at a postgraduate level. I also want to give thanks to God; without God, things would not have been possible. While it is not always easy to juggle work and school, as well as other pressures in my personal life, I am encouraged by the work. Seeing the connections and areas of need gives me resilience and the desire to keep doing what I am doing. In my Masters of Social Work, I have realised that I am the right person for the social worker’s role.
Vicky Opia
Studying a Masters of Public Health in Gulu, Uganda
I am in my first semester and my studies are going well. During the weekend classes, we have been studying areas like research, biostatistics, epidemiology, and public nutrition. My papers and work completed so far are receiving good marks, and I am eager to incorporate issues related to prevention at Peace Hospice Adjumani. I am interested in prevention especially in the communities we work with in home hospice care, as I have been observing similar factors in some of the chronic illnesses presented, including cancer. Peace Hospice Adjumani and my studies are also correlating in an area of my course research, where I am planning a research methodology in refugee and host communities.
The last few months have been so busy. There has been partnership work we’ve been doing with the Ministry of Health (Adjumani Hospital) and with Peace Hospice Adjumani to provide community health. I am also a Rotarian, and so we are planning a cancer run on November 25 as a Rotary Club. This cancer run is to raise awareness, support current patients with cancer and their families, and to fund those who need to travel to Kampala to visit the Uganda Cancer Institute or Mulago Hospital. In addition to all this, we are still keeping in touch with the Village Health Teams (VHTs) that were trained in palliative care. We invite more partnerships and activities in the future, and are so very grateful for the support from Cairdeas IPCT.

Between classes, he takes a selfie with a fellow nursing student: Godfrey Oziti.

Phillip Amol Kuol at Arua Christian University. In the past, Phillip had online classes but now he is attending in person.

Toko Friday Santiago advocating for PcERC, our partner in hospital-integrated palliative care at a Charity event this November.

We congratulate Vicky Opia for beginning her first semester as a Masters student in Gulu University.
Compassionate Leadership Fellowship in India … Coming soon!
![]() Hannah Ikong
Hannah Ikong
![]() 9th November 2023
9th November 2023
Inspire, Empower, Influence and Transform: this is the approach to mentor the next generation of palliative care leaders in India. In the above video for the October 2023 "Cairdeas Gathering," Dr Chitra Venkateswaran, Cairdeas IPCT Lead in India introduces the fellowship plans and work completed by herself, Dr Mhoira Leng and the rest of the steering group.
Alongside partners Believers Church Medical College Hospital (BCMCH), Global Health Academy (University of Edinburgh), Indian Association of Palliative Care (IAPC), and the RMD Trust, Cairdeas IPCT is proud to support this year-long advanced leadership programme.
Planning for the programme is quite well underway. In person meetings were conducted over the first week of October to finalise all content details and logistics. This has lead to an agreement with BCMCH to host the in person trainings for the fellowship, providing fellows and faculty with accommodation and a meeting hall.
The curriculum for the programme has been designed and tested in other international fellowships by steering group members Drs Mhoira Leng and Chitra Venkateswaran. Currently, there is a call for applications, from now until the 7th of December, for those practicing palliative care in India.
Cairdeas IPCT will be supporting the programme in purchasing assessment tools, assisting in faculty travel logistics and providing administrative support.
The Fellowship is scheduled to begin with a week of intensive training at BCMCH, Thiruvalla, Kerala from February 18th to 25th, 2024. There will be follow-up online sessions every month, and another in person training in February 2025. Mentors will guide the fellows and work together online and in person during the fellowship.
For further information, please visit the IAPC website for a detailed course description, official letter, and brochure. You can also email the fellowship administration team at clfellowship.india@gmail.com.

Steering group includes (left to right) Dr Leejia Mathew, KV Ganpathy, Dr Mhoira Leng, Dr Republica Sridhar, Dr Chitra Venkateswaran, and not pictured: Dr Savita Butola and Dr Rajam Iyer.
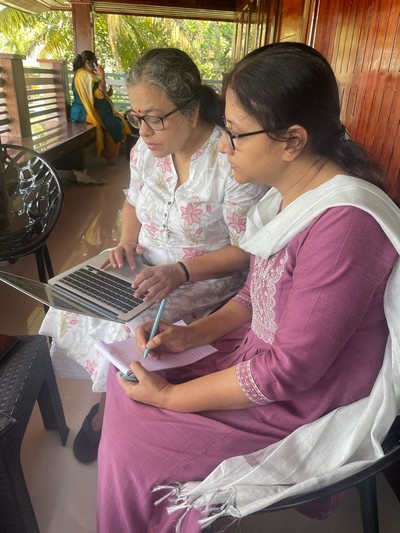
Fellowship logistic planning between Dr Chitra Venkateswaran (left) and Dr Leejia Mathew (right).

Planning over World Hospice and Palliative Care Day (WHPCD) -- wearing blue! -- Dr Chitra Venkateswaran (right) and Dr Mhoira Leng (left).
From the beginnings to tomorrow: Journey through Uganda
![]() Hannah Ikong
Hannah Ikong
![]() 27th October 2023
27th October 2023
Journey to Uganda: the summer month’s fundraiser for partners in Uganda is officially closed and we thank all who supported us in #BuildingaWorldthatCares.
We’ve enjoyed each part of the trip together, from interactions on our fundraiser WhatsApp groups to the engagement on our website and Just Giving. Wait, that’s not all: the trip began much earlier than this when Cairdeas IPCT first began working in Uganda.
Fifteen years ago, Dr Mhoira Leng and newly appointed Dr Liz Namukwaya partnered with the newly developed hospital-integrated palliative care unit in Kampala, Uganda. She was asked to lead the development for the unit’s academic activities, which involved Makerere University and the Mulago National Referral Hospital.
This is how the Mulago Makerere Palliative Care Unit (MMPCU) was formed to become a leader of palliative care education and training, research, advocacy, and clinical service provision. In 2017, the MMPCU developed an NGO arm called PcERC (Palliative care Education and Research Consortium).
We have been able to replicate the unit in Kiruddu National Referral Hospital and further educational activities with flipped classrooms, video resources, and an upcoming specialist medical fellowship. Cairdeas IPCT is proud to work with the unit – MMPCU / PcERC – further palliative care in Uganda.
From our first joint partner came the second: Vicky Opia, now Executive Director of Peace Hospice Adjumani met Dr Mhoira Leng and their unit as she attended their nurse leadership fellowship eight years ago. Cairdeas IPCT was eager to join Vicky’s growing hospice organisation and support her passion for palliative care for the marginalised in refugee and host areas of Adjumani district.
As collaborators we have accessed the needs of those around Peace Hospice Adjumani, provided trainings in palliative care, and supported the community hospice to reach more patients and families.
The 2023 fundraiser of Journey through Uganda has been years in the making and it was a joy to collect the photos, videos, and interviews that made up the website’s virtual journey.
Through our work together, hundreds of healthcare professionals have been trained and implemented palliative care in their own setting, with thousands of patients and their families receiving quality and compassionate care.
It’s not too late to check out our virtual Journey through Uganda! Keep an eye out for new blogs (be notified here for new posts) and travel with us together into our next years of palliative care for all.

Our virtual Journey through Uganda was not always on foot! We traveled by plane, boat, motorcycle (boda) and car across the country.

Members of the PcERC team snap a picture during daily walks.

Wide open spaces in Adjumani district, shared by Vicky Opia, Executive Director of Peace Hospice Adjumani.

Thank you for joining us on the journey! Pictured here are the January 2023 team of researchers in Dama village, Obongi district.
