
Blog: Specialist Need for Palliative Care: Report from 8th Annual ESCACOP Conference
![]() Hannah Ikong
Hannah Ikong
![]() 24th October 2023
24th October 2023
It was a pleasure to speak with Dr. Peace Bagasha, a kidney disease specialist working at Mulago Hospital and pursuing a PhD, on quality of life of patients with kidney failure in a national referral hospital in Uganda, at Makerere University. She is also the board chair of our partner institution, Palliative care Education and Research Consortium (PcERC) and a member of the Palliative care Specialist Fellowship Programme (PcSFP) steering group, which is working to provide specialist training to doctors in Uganda and beyond.
Last month, Dr. Bagasha represented this steering group at the 8th Annual East Southern Central African College of Physicians (ESCACOP) Scientific Conference and Annual General Meeting, and gave a talk on the work done to develop and implement potentially the first palliative care fellowship program in Sub-Saharan Africa. I was eager to talk to her about her conference experience, feedback received about the presentation, and any insights on incorporating palliative care fellowship program into ESCACOP.
With many thanks to Cairdeas International Palliative Care Trust for the travelling grant, Dr Peace was able to fly to the beautiful Elephant Hills Hotel in Victoria Falls, Zimbabwe where the conference had been organised. Whilst on a layover at Addis Ababa airport in Ethiopia, she bumped into a group of seven other Ugandans heading to the same conference. They represented many other specialities, including infectious diseases and Cardiology, but in the airport – and the later at the conference – she noted there were hardly any palliative medicine doctors.
This gap in palliative medicine specialists influenced Dr Peace’s speaking arrangements at the conference. Her first presentation entitled; “Lived experiences of patients with end stage renal disease in Uganda”, a result of her PhD work research, raised many questions on the interplay between what “should” be done for patients with kidney failure in resource limited settings and what “can” be done given the prevailing circumstances. She presented “palliative care” as what is done but “we do not acknowledge that we are doing it.”
She noted that; “Before I spoke, I was introduced by a fellow nephrologist, the session chair, and in her introduction, she said, ‘I don’t know what the connection is between Palliative care and Nephrology, but I look forward to finding out’”. Because of his comment, Dr. Peace realised the need to present palliative care from the basics and particularly emphasis its vital role in non-cancer chronic illness including nephrology.
Due to this first presentation and the questions regarding palliative care, she revised the sedond presentation which was on the PcSFP. “I realised that we had taken it for granted that everyone knew what palliative care was when preparing for the conference … so I introduced the concept into our presentation, including its place in the overall health system, various palliative care models, and levels of service integration.”
Dr Peace explained: “The conference was essentially for internal medicine physicians from different specialities, so the idea that palliative care was to be practiced in internal medicine was, to most people, something that they hear about in theory but they don’t actually practice. Many physicians practising in Africa consider palliative care as a foreign concept; a model only to be done in foreign countries where they have an excess of money and resources.”
She continued: “So what I did was show them that they practice palliative care in the care they provide every day. I began my talk by asking the attendees, how many of you ask what symptoms does your patient have? How many of you treat the symptoms that they have? In a way, all of them practice palliative care as they alleviate distress and reduce symptom burden and for many, this was a real eye opener.”
During the time of questions, Dr Peace was able to address concerns about doctors speaking about death and providing advance care planning for patients. “In the African culture, talking about death is a taboo; many rather keep quiet and then when it happens, they deal with the death. If we could give the conversation a chance, then the benefits are enormous. We have land wrangles as we don’t have lawyers routinely making wills for people, and we have a lot of grief and bereavement where families are falling apart. If we would talk about death before it happens, it would avert a lot of misery.”
Dr Peace wouldn’t go as far to say that she completely changed the conference attendees’ perspectives on palliative care, but she recounted that “they went away with something to think about. They said that they embraced the programme, and if we do develop a fellowship, we can count on ECSACOP.”
In particular, the PcSFP was accepted by those at the ECSACOP conference leadership. Once they understood the role of palliative care in patient care and in the overall health system, they recognised that this fellowship would fulfil the specialist need on multi-disciplinary teams. Even the conference leadership spoke, indicating support for the programme.
Well, what is to be done next? When I asked Dr. Peace this, she gave me two thoughts. First, we can work together to integrate specialist palliative care into the ECSACOP training programme for internal medicine. These internal medicine fellows study many other sub specialities, such as cardiology, nephrology, and infectious diseases, and so palliative care can be included in their rotations.
Secondly, she suggests that the PcSFP could be added to ESCACOP as one of their new speciality fellowship options. As we continue to work together, we can utilise the ESCACOP model, of using any accredited hospital as a training site, to maximise training opportunities. The fellows would converge together from the different sites and countries of ESCACOP for the major exams, yet otherwise they would work in their local accredited training hospital sites under supervision of the specialist physician. Later, graduates of this fellowship programme would train new fellows. This would lead to more training oppotunities, ultimately leading to increased accessibility and affordability of such fellowship training that is currently out of reach for the majority.
We are looking forward to seeing how the PcSFP can partner with ESCACOP to reach more physicians in sub-Saharan Africa. We are grateful to Dr Peace Bagasha for her representation of the steering group for our developing fellowship, and for advocating for palliative care in every health system.

Dr Peace Bagasha represented the steering group from 31st August to 2nd September 2023 at the 8th Annual ESCACOP Conference in Zimbabwe.

Dr Peace pictured in the far right (yellow) at the conference venue.

Dr Peace added to the presentation, explaining the need for palliative care and such a programme.

Snapshot of Dr Peace presenting during the conference.
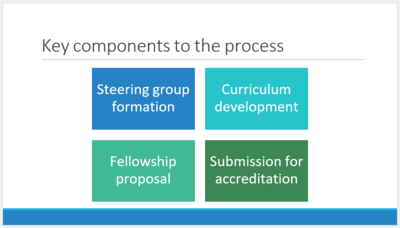
Presentation slide created by Dr Kate Howorth in 2022 and presented by Dr Peace Bagasha. Much progress: we are now in the last box of submission for accreditation!

Grateful for Dr Peace's opportunity to present and network with other sub-Saharan physicians at the 8th Annual ECSACOP Scientific Conference.
