
Blog: Integration of palliative care into healthcare provision for South Sudanese refugees and host communities in Adjumani and Obongi districts of Uganda, By Elizabeth Nabirye
![]() Cairdeas
Cairdeas
![]() 3rd November 2021
3rd November 2021
Empowering communities and health systems to address health related suffering in host and humanitarian settings through capacity building and integration funded by UKAID.
Background
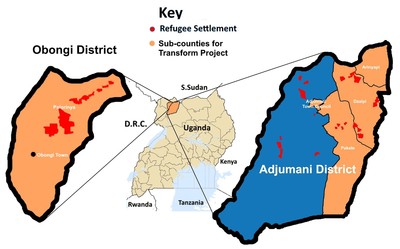
Palliative care (PC) is rarely prioritised or integrated in humanitarian settings and so evidence is needed from field settings to inform integration of PC in health systems. Uganda is the 3rd largest host for refugees globally, and previous work with Ministry of Health of Uganda (MOH), Peace Hospice Adjumani (PEACHOA), Palliative Care Education and Research Consortium (PcERC) and Cairdeas (IPCT) to integrate PC in Adjumani district, with a population of 210,000 refugees, 240,000 hosts) included training of Village Health Teams (VHTs) and Healthcare Workers (HCWs). This is now being extended to the new Obongi district with a population of 120,000 refugees and 50,000 hosts.
Rapid Systems Appraisal (RSA):
A RSA was conducted with the aim to evaluate the setting and systems affecting chronic diseases and health related suffering for refugees and host populations in both Adjumani and Obongi districts.
The methods:
This included documentary review, mapping of key stakeholders, observing of practice, qualitative interviews with 4 groups of informants: patients and their caregivers, palliative care providers, key opinion leaders; MOH, humanitarian stakeholders, community and healthcare workers.
The broad themes following thematic coding and analysis of 40 interviews included
- Health system issues; planning, resources, capacity, pathways of care, integration
- Understanding of palliative care
- Education and training
- Impact of palliative care
- Challenges and gaps
- Community and HCW experience
- Culture and stigma
Results:
Health system issues; these included issues relating to planning, resources, capacity building, pathways of care, integration
“There are a few things that can make you be able to integrate palliative care; One is ownership...it is not a peace hospice project but an Obongi district government programme. Ownership goes with leadership... the members for health need to take the leadership.” Hon Dr. MP
“At community level it is only one person and this remains a challenge. …plan for the future of palliative care strategically… so that there is no gap in patients care” UNHCR
“At the Humanitarian aspect, the time of making proposals to the funders on what they are going to implement, the picture is of comprehensive health care, which is always sent out but palliative care may not come out pronounced and there is need to have that strong advocacy of this component. There is time for all this to change through advocacy and training” Dr MTI
Understanding of palliative care and planning
"I thought palliative care was last office. Where there is nothing we can do and we just care for them, as they wait for their own death and I never thought this would need any technical person." Health worker
"Palliative care is like manna from heaven’ ‘I pledge to include it in district strategic planning’" RDC
"Palliative care is very important...it has touched my heart…this programme is the best investment for so far because it prepares the heart of the people ...we are answerable in future, when I was sick and bedridden you gave me care....’" Community leader
"There are so many people in the community with chronic illness but by the time we discover them, it is too late so we need to create awareness and also embrace palliative care’" DHO
Education and training
“One of the challenges is the skilled staff to give the services, a few staff who have been trained and even commitment is a challenge
Doing capacity building training is very important....training and skilling primary and secondary care ...but also include leaders so they know what is being implemented.” Health worker
"VHTs, they are really so useful in the community because they can identify any condition, report and refer. So building the capacity of the VHTs is very important, and the component of research is equally very good, it gives evidence.’"Health care leader
Community experience
"We need to work together and be on radio to share. People can be abandoned mostly because of ignorance...people think someone who is sick can infect them...such as cancer. This programme is the best investment, so far because it prepares the heart of the people’"Community leader
"But our communities here thinks that when someone is very sick, they should be cared for in the hospital and die from hospital, so taking them home is considered to be a taboo’" Health care leader
"We thank our Almighty God to have given heart to the people of this organisation to come and us...this is God’s love to our district...without God’s love they would not come this way’" Faith leader
Impact of Palliative care
"So whenever I pay a visit, it’s like am bringing glory to their home. We really smile, we really laugh so whenever we are in that community, they are really appreciating our service and always tell us that without us, they would have not lived up to this time. That is encouraging. So they are really pleasing me so much, I bring hope to them, but when I lose one, I’ve also lost hope too.’" PC worker
Challenges and gaps
"Facilities don’t have morphine and other drugs but also health workers need to be trained to be able to assess these patients and manage their symptoms." Health worker at health centre III
"Because I lack the knowledge, I just don’t even attend to them, I just refer them to other Health care workers As health workers we sometimes do little to help these patients with chronic illness, for example at times their symptoms are so complex that we can’t manage them because of knowledge gap." Health worker at health centre II
"These patients have a lot of symptom burden especially pain which is always uncontrolled with available pain killer that we give them. Available pain killers include Paracetamol and diclofenac at times ibuprofen. We don’t have morphine at our facility. " Medical Clinical Officer
Culture and stigma
"But our communities here thinks that when someone is very sick, they should be cared for in the hospital and die from hospital, so taking them home is considered to be a taboo that is the other challenge " Doctor
"When they have chronic illness they can’t support themselves, but also the refugees have different cultures and this can be a problem taking care of them, some use their local herbs." Nurse
Conclusions:
PC service integration is needed and previous interventions were effective but we need to extend to all aspects of planning and implementation.
Refugee and host communities must have ownership and the services should be tailored to the community needs.
Further evidence on the PC needs will be collected including novel tools to understand community experience.
A comprehensive education package for HCW, VHTs and family caregivers and community mentors will be implemented and evaluated.
Acknowledgement
Many thanks to those who participated in this RSA which was led by Dr. Mhoira Leng, Elizabeth Nabirye, Vicky Opia, Godfrey Oiti and the entire PEACHOA team. Special thanks to all our participants (patients and families, VHTs, Health works, opinion leader) and funders.

Setting of Obongi district

During an observation visit of a palliative care health worker with a patient

Interview with people (VHT) who interact with patients with chronic illness

Leaders of the programme across the Nile
