
Blog: “I wish palliative care could be like malaria.”
![]() Hannah Ikong
Hannah Ikong
![]() 26th January 2023
26th January 2023
– Simon Maku, clinical officer, volunteering in Peace Hospice Adjumani (PEACHOA), Uganda.
This was the first time Simon Maku ever completed a Needs Assessment, a type of data collection tool to determine the exact medical and social conditions of those living with palliative care needs in a certain area. It was also my first Needs Assessment in rural Northern Uganda, and I learned quite a bit with the traveling medical team and community-based Village Health Teams (VHTs).
Our traveling team of five included Dr Mhoira Leng, in addition to Vicky Opia, Godfrey Oziti and Simon Maku from PEACHOA, and Toko Friday and myself from the Palliative care Education and Research Consortium (PcERC). We were very happy to work with a team of thirteen VHT mentors and VHTs, who connected us to each individual and family and often served as translators.
You might be wondering what is involved in a Needs Assessment? Of course, we are to collect data, but there’s something to be said on how it is completed and its connection to the bigger picture of developing quality palliative care for all. Our recent one was in Obongi district of Northern Uganda from the 5th to 8th of January when it was not too hot (nor rainy).
The data collection work started weeks in advance with the support from our administrative teams and Godfrey, who did an excellent job coordinating the VHT Mentors and VHTs. From our records, in some three villages in Obongi district (Dama, Bongilo, and Pasu), there was 126 individuals identified in advance by the VHT Mentors and VHTs with possible palliative care needs. With much teamwork and effort, we visited 117 of these individuals in their own homes.
Let me just pause for a moment: over a 4-day period we met and screened 117 people (almost 30 a day!) for palliative care needs. And even if they did not have a chronic, serious illness, we always took a moment to listen and counsel, share medical advice, and perhaps write a referral to a nearby health centre for further investigations and care. Those who did have palliative care needs were given a more detailed assessment, often with a lot of translation support, and some 81 individuals were then recruited to the Needs Assessment study.
Yet this was more than “a study,” I felt many times during the trip, this was getting to know each individual as a person, not a patient. Some spoke about their children who have died, or their husbands out of country. Others did not speak much but created beauty with artwork on the walls and maintaining beautiful, trimmed hedges around their home that spoke of better times. There was also a lack of food (tight rations) and eating one meal a day could be struggle.
One particular gentleman I visited with Toko Friday was a retired teacher from South Sudan. In addition to having cancer of the throat, he had others issues with his refugee status, which greatly affected the care he could receive at local and national health centres. Thankfully our team was to connect with those who handle refugee statuses as well as look into what kind of oncology support that he could receive, and we know that the VHT Mentors and VHTs will continue to liaise with and support him.
I found the Needs Assessment trip to be the bridge between the deep connection of humanity and suffering and the call for health system changes.
One moment, we were meeting one-on-one with someone like the retired teacher who had many levels of need but couldn’t stop smiling and cracking a joke or two about oncology doctors, while other times we sat with worried family, who had many questions for us, including inquiries about getting a wheelchair for their child who has a complex disability.
We saw the needs in the data collection even: initial findings report that a third had neurological conditions (acquired brain injury, complex and learning disabilities, Parkinson’s, etc.) with many others live with HIV/AIDS and musculoskeletal or chronic pain. These serious, chronic illnesses took a toll on the individual and their family, with high levels of distress reported, as well as the inability to work or perform daily tasks.
Our advocacy has begun to make palliative care as common as malaria. Even during our trip, we shared our Needs Assessment work and initial findings with the Obongi District Health Official (DHO) Mr Dominic Lomurecu.
Mr Lomurecu was already aware of and supported our activities, recognising the need for quality, accessible palliative care in Obongi district. He was in favour for more training of palliative care in Northern Uganda, which included communicating to other stakeholders about the unmet needs and how we all can integrate palliative care in all the health services.
Readily identified and accessible care, with widespread education and desensitisation from the healthcare workers to VHTs to the family caregivers, is a global palliative care need. Just as outbreaks of malaria demand a response from various organisations – i.e., to control the mosquito population, provide care for the ill, and educate the community – so does the need for palliative care must be met by many stakeholders in multiple levels.
And our time of Needs Assessment in places like Bongilo, Dama, and Pasu villages in Northern Uganda did confirm quite several unmet palliative care and psychosocial needs.
Please stay tuned for further updates in this work of creating quality, accessible palliative care. We will be sharing more blogs soon about the VHT Mentors and VHTs and how it is to live in fragile setting with palliative care needs.

The start of the Needs Assessment: the traveling team has just reached Obongi town after a 12-hour trip from Kampala, Uganda.

Snapshot of the Nile River, which divides Obongi district from Adjumani district.

Screening individuals for the Needs Assessment is an all-day process. Dr Mhoira hence took to a motorbike (boda boda) with driver Emma.

VHT mentors, VHTs, boda boda drivers, PEACHOA, PcERC and Cairdeas all played a role in the data collection, pictured here in Pasu village.

Getting to know the person behind the diagnosis: for one individual, she showed off her beautiful trimmed topiary.

A quick break of the whole team under a grove of trees: connections were built within the team as well as within the community.
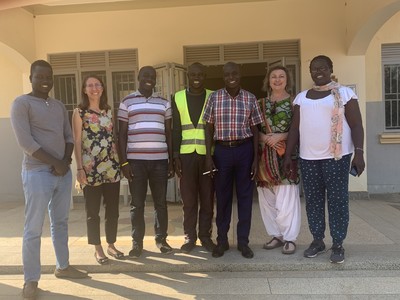
Pleased to stand with Mr Dominic Lomurecu, the DHO of Obongi district and a strong advocate for palliative care. Pictured left to right: Simon Maku, Hannah Ikong, Toko Friday Santiago, Godfrey Oziti, Mr Dominic Lomurecu, Dr Mhoira Leng, and Vicky Opia.
