
Blog: An Overview of the 2018 Global Palliative Care Day - Presentations Now Available
![]() Cairdeas
Cairdeas
![]() 16th January 2019
16th January 2019
A fairly typical cold and wet November day in Edinburgh was significantly brightened for all those who attended the Global Palliative Care Day in St. Catherine’s Argyle Church on the south side of the city. Jointly organized and run by Cairdeas, The University of Edinburgh’s Global Health Institute and the International Children’s Palliative Care Network (ICPCN), it wasn’t simply the scope of the presentations that made it ‘global’, but the participants from nine different countries, who represented cutting edge palliative care research, policy, and practice from around the world. Delegates from the UK included primary healthcare researchers, palliative care (PC) Registrars (from London, Manchester, Newcastle and Glasgow), students completing their Masters Programmes in areas related to PC, and GPs and Consultants with specialisms in PC.
Professor Julia Dowling focused on the five key messages of the Lancet Commission Report stressing that, in keeping with the call for universal access, palliative care is notan optional extra. Given Julia’s background (ICPCN) she understandably has an emphasis on the palliative care needs for children, telling us that $1 million would cover the morphine needs for children globally, a paltry figure in today’s million pound budgets.
Some of the most memorable moments of the day came from the real life stories that were told by in-country doctors such as Dr. Mhoira Leng, Medical Director of Cairdeas. Mhoira told us about Diane, who had end-stage organ failure and leg lesions and was receiving medical treatment in Kampala. Restricted to a hospital bed, the most important thing for Diane was that she didn't feel abandoned and that she had someone to talk to. Mhoira told us, “Palliative Care means dignity, and treating Diane as a whole person gave her the dignity she needed.” Dr. NahlaGafer, who works in Sudan, had similar stories to tell, relaying the words of one patient who told her, “when I come to the clinic, I feel like I am not a sick person – I feel like I am coming to meet my friends.”
In the context of global news, we constantly hear about refugees being refused entry at borders, turned away, ‘contained’, or shunned. It was heart-lifting, therefore, to listen toDr. Gurswan Purewal present on the her work with the refugee population in Adjumani District in Uganda. She spoke of how the local population welcomed the refugees, referring to themselves as the ‘host’ population and calling the refugees’ region as a ‘settlement’ as opposed to a ‘camp’. But behind the semantics, there lies a very real sharing of heath and social care resources between the host population of 240,000 people and 260,000 refugees – would that we were all so sharing.
The following is a list of the presenters and the topics on which they spoke:
Prof. Julia Downing– Severe Health Related Suffering - a new paradigm in Lancet Commission Report;
Dr. Sebastian Moine– Astana and Palliative Care;
Dr. Mhoira Leng- 10 year evidenced based review from Makerere University and Mulago Hospital (MMPCU), Uganda;
Dr. Dan Munday – Developing and implementing the SPICT-LIS;
Dr. Nahla Gafer– Pioneering palliative care in Sudan;
Joy Kemp– Palliative care and midwifery – commonalities in health partnerships,
Appraisal in the refugee population in Adjumani District in Uganda;
Dr. David Fearon– pioneering palliative care in Mauritania;
Dr. David Butler -PRIME UK Teaching palliative care in different settings; cultural issues;
Dr Gursaran Purewal- Rapid Systems Appraisal in the refugee population in Adjumani District in Uganda;
Dr. Laura Tupper - Lessons from Chile.
All of the presentations have been made publicly available under the resources section of the Cairdeas website – for quick reference follow this link.
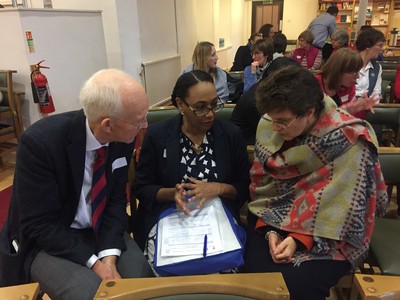
Professor Scott Murray, Dr. Nahla Gafer and Professor Julia Dowling deep in conversation during a break in proceedings

Dr Mhoira Leng and Professor Liz Grant

Dr. Sebastian Moine making his presentation
